Metabolic Bone Disease 2009
advertisement

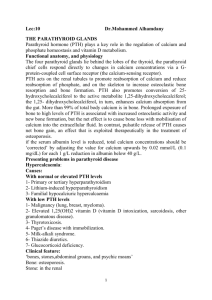
Metabolic Bone Disease Douglas Stahura DO 19 March 2002 Overview Normal bone undergoes constant remodeling: – Production of organic matrix (osteoblasts) – Matrix maturation – Mineralization of mature matrix – Osteoclastic resorption of mineralized bone Overview Metabolic bone disease refers to : – Diffuse decrease in bone density (osteopenia) and strength – Due to: – Increased bone resorption – Decreased bone formation Overview Examples – Osteoporosis - decreased bone mass in combination with disruption of normal architecture – Osteomalacia – disorder of mineralization of newly formed matrix – Hyperparathyroidism – chronic excess of PTH leads to marrow fibrosis, woven osteoid, expansion of osteoid surface, increased collection of osteoclasts Renal Osteodystrophy Spectrum of disorders that include: – Osteitis fibrosa – increased bone turnover – Adynamic bone disease – low turnover – Osteomalacia – defective mineralization All related to disorders of: – Mineral ions Ca++, PO4--, Mg++ – Parathyroid hormone (PTH) – Vitamin D metabolism Epidemiology Sherrard,Hercz Kid Int 1993;43:43642 Clinical Features Musculoskeletal – Bone Pain - in advanced renal/severe bone Low back, hips, legs aggravated by weight bearing Acute localized pain Periarthritis with deposition of calcium phosphate crystals Gradual onset muscle weakness Axial bone fractures – small increase in axial/hip fractures Clinical Features Pruritus – common in hemodialysis Metastatic calcification – Extraskeletal – aggravated by persistently elevated Ca x P product Most commonly found in the arteries Calciphylaxis Syndrome characterized by skin necrosis that is attributed to medial calcification of small and medium sized arteries Possible depression of Protein C activity causes vessel thrombosis Manifests as painful violaceous lesions with peu d’orange changes, often symmetrical with involvement of the trunk and extremities Commonly progress to superficial ulceration, necrosis, and infection Calciphylaxis Calciphylaxis Histology Pathogenesis of Renal Osteodystrophy Role of Phosphorous retention Role of Calcitriol replacement Role of parathyroidectomy Phosphorous and Calcium Phosphate – found as a mineral and as a ester Widely found in milk products, meat, eggs and cereal Phosphorous and Calcium Na+/Phosphate cotransport major route of absorption Calcitriol stimulates Na+/Phosphate function Hyperphosphatemia directly suppresses calcitriol production Phosphorous and Calcium Kidney eliminates phosphate in amount equal to GI absorption 5-20% of filtered load is excreted In renal failure (loss of nephron mass), ultrafiltered load goes up, Tubular reabsorption goes down, and fractional excretion of phosphate can reach 60-90% until GFR falls to <25 ml/min Phos excretion in kidney is stimulated by PTH, but limited by total GFR. Vitamin D Metabolism Phosphorous and Calcium Ionized Ca++ level is regulated closely Regulators are: – PTH – Calcitriol ( 1,25- dihydroxycholecalcif erol) Phosphorous and Calcium Calcitriol binds to VDR and increases the activity of calbindin D9k and CA++ ATPase Paracellular transport is greatly increased in the presence of CITRATE Paracellular transport not affected by ACETATE. In renal failure Hyperphosphatemia due to reduced nephron mass – Reduces Ca concentration – Suppresses calcitriol production directly – Reduces the sensitivity of parathyroid to inhibition by calcitriol Hypocalcemia stimulates PTH – Maintenance of Ca level with exogenous Ca does not prevent hyperparathyroidism Decreased responsiveness to Calcitriol – Normal levels of calcitriol cannot suppress PTH possibly due to downregulation of VDR receptors – Monoclonal expansion of parathyroid cells/nodular adenoma = tertiary hyperparathyroidism Skeletal resistance to PTH Chronic metabolic acidosis Phosphorous and Calcium Phosphorous and Calcium Slatopolsky, Bricker Kid Int 1973;4:14 Recent Investigation Martinez, Llach Neprol Dial Transplant 1996,11:22-28 Recent Investigation Calcitriol Replacement Calcitriol therapy for advanced and endstage renal disease and iPTH> 200 pg/ml – Calcitriol superior to Ca alone in suppressing PTH – Prevention of hyperparathyroidism is key to minimizing metabolic bone disease – Calcijex(IV), Rocaltrol(po) Phosphate Binders Target Ca++ level 7.5-9.5, Phos 3.0-5.0 minimize hyperphosphatemia by use of phosphate binders CaCO3 – Tums CaAcetate – Phoslo Sevelemar – Renagel, Renvela Lanthanum Carbonate - Fosrenol Aluminum hydroxide - alternagel only for severe cases for short term control only! Magnesium Oxide - Magox (watch Mag level!) – Up to 2.5 gms elemental Ca/day tolerated Calcitriol Replacement – Must control serum phosphate levels <6 mg/dl to prevent metastatic calcification – Therapeutic endpoint is iPTH between 130-195 pg/ml – Adverse side effects are hypercalcemia, hyperphosphatemia, possibly metastatic calcification – PTH <100 could set pt up for adynamic bone disease which can also cause hypercalcemia (not a typo- hypercalcemia). Calcitriol Replacement Vitamin D Analogs – Hectorol (doxercalciferol) PO or IV – Zemplar (paracalcitol) PO or IV – Paracalcitol produces less hypercalcemia or hyperphosphatemia, much more effective than Calcitriol. Calcimimetics New treatment for secondary hyperparathyroidism: – Sensipar (30-60-90 mg pills) – Binds to receptors for calcium in the parathyroid cytoplasm. – Potent suppression of PTH – Rare hypercalcemia (but it still happens) Parathyroidectomy Severe Hyperparathyroidism – – – – Tertiary (iPTH > 700) Or refractory hypercalcemia… Or refractory hyperphosphatemia… Despite adequate therapy Secondary Hyperparathyroid – With refractory symptoms (pruritis), or – In transplant candidate PTX is Rare since the introduction of Zemplar and Sensipar. Treatment References Comprehensive Clinical Nephrology, Johson 2000. Atlas of Physiology, Despopoulos 1991. Llach et al, Secondary Hyperparathyroidism in Chronic Renal Failure: Pathogenic and Clinical Aspects, AJKD;38;5,Suppl 5, s20-s33. Clinical Physiology of Acid-Base and Electrolyte Disorders, Rose, 2001 Harrison’s Priniples of Internal Medicine, 14th Ed Martin et al, Vitamin D Analogs for the Management of Secondary Hyperparathyroidism, AJKD;38:5, Suppl 5, s34-s40.