Children`s Respiratory Disorders
advertisement
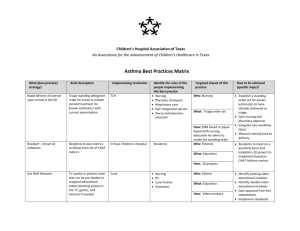
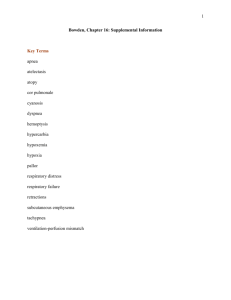
Children’s Respiratory Disorders Epiglottis - RSV/Bronchitis - Pneumonia Asthma - Cystic Fibrosis Marydelle Polk, Ph.D., ARNP-CS Florida Gulf Coast University Objectives Describe factors that influence the etiology and course of respiratory infections in children. Differentiate among Epiglottis, RSV/Bronchitis, Pneumonia, Asthma, and Cystic Fibrosis in terms of etiology, defining characteristics, and nursing management. Respiratory System The respiratory system permits ventilation through the process of inspiration and expiration Respiratory Infections Influencing factors * Age * Anatomical Size * Resistance * Seasonal Variations Etiology * H. influenza, Group A -Hemolytic Streptococcus, Staphylococci, Chlamydia trachomatis, Mycoplasma, pneumoccoci Epiglotitis Definition A severe bacterial infection which causes inflammation of the epiglottis and surrounding areas. Incidence Usually occurs between the ages of 2 – 5 years of age, but can occur from 7 mos. – 11 years – rarely to adulthood. Epiglottitis History Abrupt onset – History of pharyngitis. Clinical Signs & Symptoms Wakes up looking very ill, fever, sore throat, dysphagia, drooling, dyspnea, “dog position.” Epiglotitis Clinical Signs & Symptoms * Anxious/apprehensive * Muffled, froglike croaking * Quiet inspiratory stridor Always observe for the absence of cough, drooling and agitation – hallmarks of epiglottis. REMEMBER !!! 1. Never examine the pharynx. 2. Leave the child in a sitting position – preferably in parent’s lap. 3. Child is anxious – Do not cause further distress and never leave the child alone. 4. Cyanosis is a late sign of hypoxia (PO2 < 50). Nursing Diagnoses Ineffective breathing pattern r/t inflammatory process. Fear/anxiety r/t difficult breathing and unfamiliar place/procedures. Nursing Coventions Observe for progressive worsening of respiratory status. Prepare for tracheostomy. Be prepared for administration of O2, IV antibiotics, sedation. Monitor VS, LOC, O2 levels, fluid status. Provide calm reassuring support to child and parents. Prevention is via the H. influenza B vaccine. Nursing Coventions Administer antipyretic medication, tepid sponge baths, or cooling mattress if indicated. If needed, provide cool mist for humidifying air. Ensure adequate rest and provide a less stressful environment. Organize nursing care to give adequate rest periods. Early Epiglottitis Note the tripod (dog-like) position and the leaning forward Progressive Epiglottitis Bronchiolitis Definition – An acute viral infection primarily occurring at the level of the bronchioles. Etiology – Respiratory Syncytial Virus (RSV). Subgroup A > B in children developing bronchiolitis and pneumonia. Incidence and Transmission * URI of the infant – 2-5 mos. Rare in children over 2 years. Considered to be the most important pathogen in the infant. Usually preceded by a viral URII (RSV). * Increased incidence due to (1) direct contact – hands, eyes, nose, mucous membranes and (2) the virus has a long life span. Clinical Manifestations Mild (Initial phase) * * * * Rhinorrhea Pharyngitis Coughing and sneezing May present with ear or eye infection * History of intermittent fever Clinical Manifestations Moderate (Progressive) * * * * coughing and wheezing Air hunger and WOB Tachypnea and retraction Cyanosis Sternal Retractions When an infant/child is retracting like this – what else would you observe? Clinical Manifestations Severe * * * * * Tachypnea > 70 breaths/minute Listlessness Apnea spells Poor air exchange breath sounds Nursing Diagnoses Ineffective breathing r/t poor gas exchange. Altered activity level r/t work of breathing. Potential of fluid volume deficit r/t poor fluid intake. Nursing Coventions Provide humidity – cool, moist oxygen Adequate fluid intake Ongoing assessment and monitoring of O2 status, VS, activity level Possible administration of antiviral agents (RespiGam – used more for prophylactic value) Nursing Coventions Conserve child’s energy Observe for signs of dehydration: * * * * Sunken fontanel Poor skin turgor Dry mucous membranes Decreased and concentrated urinary output Remember… As this infection is due to a virus – standard Rx may not prove to be effective in non-complicated situations, including: * antibiotics * bronchodilators * corticosteroids * cough suppressants Pneumonia Inflammation of the alveoli caused by bacteria, virus, Mycoplasma organisms, aspiration, or inhalation. Types of Pneumonia Lobar – Large areas (segments) of one or both lungs are involved. Broncho – bronchioles become clogged with thick mucopurulent mucus consolidates into patches in nearby lobes. Types of Pneumonia – con’t. Interstitial – Primarily occurs within the alveolar walls and interlobular tissues. Incidence and Etiology Incidence 10-20 % of the cases of pneumonia are bacterial; 10 % are mixed – both viral and bacterial. 70 – 80 % are viral. Etiology Mycoplasma pneumoniae – most common in children 5 – 12 years-of-age. Chest x-rays - Pneumonia Clinical Manifestations fever Cough (productive or nonproductive) Tachypnea Fine crackles and rhonchi Chest pain Retractions and nasal flaring Pallor to cyanosis Irritability – restless – lethargic GI disturbances (nausea, diarrhea, pain, anorexia). Nursing Diagnoses Ineffective airway clearance r/t inflammation. Pain r/t inflammatory process: pneumonia Nursing Coventions Administer and monitor antibiotic therapy (bacterial). Monitor fluid intake, VS (especially the temperature – give antipyretics in needed (fever/irritability), bed rest, cool mist humidifier. In-hospital – monitor O2 if child develops respiratory distress. Avoid cough suppressants. Teach parents s/s of respiratory distress and dehydration. Conserve child’s energy. Reactive Airway Disease - Asthma Definition – inflammatory process of the large airways, which results in heightened airway reactivity. An obstructive disorder – due to the inflammation and edema of the mucous membranes, in thick, tenacious secretions, spasms of the bronchial smooth muscle a diameter of bronchioles. Types of Asthma Mild Intermittent Asthma * S/S 2 times per week * Exacerbations are brief * Nighttime s/s 2 times per month * Asymptomatic between episodes * Does not require chronic drug therapy * Teach and encourage parents to exposure to allergens Types of Asthma Mild Persistent Asthma S/S > 2 times per week - < 1/day Exacerbations may/may not affect exercise Nighttime s/s > 2 times per month Tx with a nonsteroidal Rx - Cromolyn Sodium, a low dose inhaled corticosteroid or a leukotriene inhibitor. Types of Asthma Moderate Persistent Asthma *Daily s/s *Daily use of short-acting 2-agonist or a low dose long-acting bronchodilator *Exacerbations affect exercise *Exacerbations 2 times per week and may last for days *Nighttime s/s > 1 time per week *May see Nedocromil (Tilade) given in children 5 years or younger in place of long-acting bronchodilator Types of Asthma Severe Persistent Asthma * Continual s/s * Frequent exacerbations * frequent nighttime s/s * PEFR and/or FEV1 > 1 second and 60 % of predicted value * Tx - high dose inhaled corticosteroids (Vanceril, Flovent) plus oral steroids as needed to control s/s Asthma Educate child and family about the disease - assist them to identify the triggers - help them in developing an “asthma action” plan AND teach and encourage child to use a peak flow meter regularly as part of his/her action plan to determine management of their s/s. Asthma Guidelines for child: 80% of child’s baseline is acceptable. 50 - 80% of child’s baseline indicates obstruction. 50% of child’s baseline indicates an acute attack. Nursing Diagnoses Ineffective airway clearance r/t allergenic response and inflammatory process in bronchial airways. Risk for suffocation r/t bronchospasm, edema and tenacious mucus. Nursing Coventions Allergy control Drug therapy Chest PT Hydration Exercise Keeping up with immunizations/flu vaccine Desensitization therapy O2 Delivery Devices Metered Dose Inhaler-Spacer Remember Assessment - Teaching - Monitoring are hallmarks of effective care for the asthmatic child - whether in an acute care facility or community health center. Cystic Fibrosis Definition An inherited, autosomal recessive disorder, which affects the exocrine glands and results in multisystem involvement. Most significant factor - The viscosity of mucus gland secretions = obstruction Cystic Fibrosis Areas of involvement * * * * Respiratory system Integumentary system GI system Reproductive system Cystic Fibrosis Major signs and symptoms due to: * Lack of sufficient pancreatic enzymes. * Gradual obstructive lung disease * sweat gland function. Nursing Diagnoses Ineffective airway clearance r/t increased mucus production. Alteration in nutrition - body requirements r/t malabsorption. Nursing Coventions Administer and monitor effects of antibiotic, bronchodilator, and nutritional management. Teach chest PT - MAINSTAY of therapy! Teach proper postural drainage technique. Promote exercise, deep breathing and directed coughing. Teach parents/child s/s of infection and complications i.e. pneumothorax Nursing Coventions Administer and/or monitor pancreatic enzyme replacement therapy. ** Always administer with meals and snacks amount given relates to degree of insufficiency and the child’s response to the enzyme therapy. Goal is to prevent FTT and to number of stools. Teach parents/child about s/s of Na+ depletion and rectal prolapse The End...