STUDENTS-RESPIRATORY_CHILD
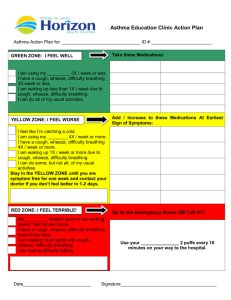
advertisement
Respiratory Disease In Childhood Nick Connolly Paediatric SpR NHS Tayside Respiratory problems in children Neonatal respiratory problems Respiratory problems in older children Chronic Acute Scenario An infant born at 30 weeks gestation develops respiratory distress at age 2 hours Respiratory Distress Syndrome Relative Surfactant deficiency 1% all births Predominantly in preterm – inverse relationship with gestation Surfactant Phospholipid Apoproteins Secreted at 30-32/40 Lack of surfactant results in atelectasis and impairment of gas exchange Production stimulated by steroids Incidence of RDS relative to gestational age 100 90 80 70 60 50 40 30 20 10 0 % with clinical RDS 26 28 30 32 34 36 Gestational Age 38 40 Further problems Ventilated Sudden deterioration requiring increased oxygen No breath sounds on the right side of chest Pneumothorax Air in pleural space Increased incidence with IPPV, CPAP and ventilation Other risk factors – RDS (stiff lungs) Spontaneous - occurs in around 1% vaginal deliveries, 1.5% caesarean sections Chronic Lung Disease Oxygen requirement beyond 36 weeks corrected gestation plus evidence of pulmonary parenchymal disease on CXR Generally follows RDS Barotrauma, volume trauma, high inspired oxygen Healing stage associated with continued lung growth over 2-3 years – often wheezy Scenario New born full-term infant with severe breathing difficulty after birth ?Dextrocardia Diaphragmatic Hernia Incidence:1/2400 Associated pulmonary hypoplasia Commonest- Posterolateral (Bochdalek), left-sided Avoid bag-mask IPPV? Respiratory support Surgical Older Children Examination Weight(length/height)..plotted! ?clubbing Chest shape Auscultation Breathing tests Chronic problems Cystic fibrosis A 1 year-old child presenting with a prolonged history of cough, loose stools and failure to thrive A newborn infant with a raised immuno-reactive trypsin level on neonatal screening who is also found to be homozygous for the ΔF508 deletion Cystic Fibrosis Autosomal recessive Carrier incidence roughly 1 in 25 people Mutations in the CFTR gene Multisystem disorder Respiratory infections are prominent Differential diagnosis Immune deficiency Ciliary dyskinesia Asthma Kartagener’s/ immotile cilia syndrome- rare Scenario NM is a 7 month old infant with cystic fibrosis who was admitted with 2 chest infections. He grew Staphylococcus aureus on his respiratory secretions Cystic Fibrosis Team Clinician Specialist nurse Clinical psychologist Social worker Physiotherapist Dietician A 7-year child presents to your clinic with a 3-month history of cough worse at night or during active play Diagnosis: ASTHMA Asthma – Diagnosis in Children SIGN Guideline May 2008 Clinical Features that increase probability: One or more : wheeze, cough, chest tightness, difficulty breathing Atopy(personal or family history) Widespread wheeze on auscultation Response to Rx Asthma – Diagnosis in Children SIGN Guideline May 2008 High Probability – diagnosis of asthma likely (trial of Rx – further Ix if poor response) Low Probability – consider Ix & ? Referral Intermediate Probability: ?watchful waiting ?spirometry(response) ? Rx & evaluate Asthma – Diagnosis in Children Management Stage 1: Treat with inhaled beta-agonists when needed Stage 2: Treat with regular inhaled steroids Stage 3A: Regular inhaled steroids + Long acting beta agonists Stage 3B: Stage 3A + Leukotriene antagonists Passive Smoking Reduces birthweight by 250g 4500 pregnancy losses p.a. 30% increase in Perinatal Mortality Teratogenic : airways, cleft lip/palate Glue ear Carcinogenic 4 million children live with smoking parent Increase likelihood of asthma attack Acute problems Acute asthma Cough and wheeze worsening over hours or days Treatment Oxygen Nebulised bronchodilator Oral prednisolone IV salbutamol IV aminophylline IV magnesium Ventilatory support Scenario 6 week old presented with increased work of breathing and possible apnoes URTI symptoms over last 2 days Bronchiolitis Viral infection – RSV Usually under 18 months old More severe in younger babies, ex prem, family of smokers Tachypnoea, poor feeding, irritating cough Apnoea in small babies Treatment is supportive Increased incidence of wheezing episodes in the next ?10 years Scenario 10 year old girl with cough, high fever and sputum production Previously very well Clinical examination: Dullness on percussion Vocal fremitus and resonance Bronchial breathing Pneumonia Neonates: GBS, E.coli, Klebsiella, Staph aureus Infants: Strep pneumoniae, Chlamydia School age: Strep pneumoniae, Staph aureus, Gr A strep, Bordetella, Mycoplasma, Legionella Scenario A 2-year old child presenting with barking cough and difficulty in breathing of sudden onset Differential Diagnosis Inhaled foreign body Laryngomalacia Epiglottitis and bacterial tracheitis Allergy Croup Croup Viral laryngotracheobronchitis Stridor, barking cough Treatment is oral steroid to reduce inflammation Scenario 9 month old infant from developing country with irritability, neck rigidity, afebrile Pulmonary Tuberculosis Mycobacterium tuberculosis Notifiable disease 1/3 of World Population! Droplet infection Prevention(of severity): BCG Drug treatment: 2 mths- Isoniazid, Rifampicin, Pyrazinamide 4 mths- Isoniazid, Rifampicin Common respiratory problems in children Infant respiratory distress syndrome CLD Congenital diaphragmatic hernia Cystic fibrosis Asthma Bronchiolitis Childhood pneumonias Croup Tuberculosis FINISHED