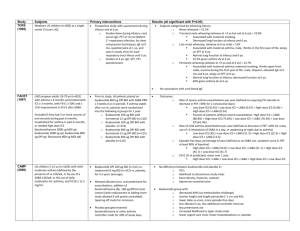
Bronchial Asthma
An Overview – Based on
GINA Management Guide Lines
Dr. R.V.S.N. Sarma, M.D., M.Sc. (Canada),
Consultant Physician & Chest Specialist
visit us at: www.drsarma.in
1
When you can't breathe,
nothing else matters®
American
Lung Association
2
Bronchial Asthma
A Paradigm Shift In
The Management
Time Now, to Unlearn Our
Age Old Outdated Practices
3
Resources Consulted – Sincere Thanks
•
•
•
•
•
•
•
•
•
GINA
ACCP
ATS
BTS
NICE
Chest Net
CDC
NAEPP
CTS
www.ginasthma.org
www.chestnet.org
www.thoracic.org
www.brit-thoracic.org.uk
www.nice.uk.org
www.chestnet.net
www.cdc.nih.gov
www.naepp.nhlbi.org
www.respiratoryguidelines.ca
5
What Is Asthma ?
Primarily – Allergic inflammation of AW
Secondary – Bronchoconstriction
– Airway Hyper-reactivity - AWHR
– Recurrent wheezing, coughing and SOB
– Airflow limitation is variable and often reversible
– Infiltration of dendritic cells, mast cells,
eosinophils and lymphocytes
6
The Huge Gap
Many patients are not detected
Many do not seek medical attention
Many have no access to health service
Many doctors do not do what is right
Stigma associated with the label
Broken marriages, alliances
Missed diagnosis (Bronchitis, LRI)
7
Mechanism of Asthma
Risk Factors (for development of asthma)
Innate Atopy
INFLAMMATION
AWHR
Airflow Limitation
Risk Factors
(for exacerbations)
Symptoms
(SOB, cough, wheeze)
Pathology of Asthma
9
Risk Factors for Asthma
Causal Factors
Indoor Allergens
–
–
–
–
Domestic mites
Animal Allergens
Cockroach Allergens
Fungi moulds
Outdoor Allergens
Host Factors
Contributing Factors
– Pollens
– Fungi, RSV
Occupational exposure
Genetic Atopy ( IgE), AWHR
Respiratory infections
Small size at birth, Obesity
Diet
Air pollution
– Outdoor pollutants
– Indoor pollutants
Smoking – Active / Passive
10
House Dust Mite
Use bedding encasements
Wash bed linens weekly
Avoid feather filled ones
Limit stuffed toys to those
that can be washed
Reduce humidity level
11
Cockroaches
Remove as many water and food sources
as possible to avoid cockroaches. Left over
food, moisture, drains, open cupboards are
the common sources – kitchen and toilets
Don’t eat anywhere except in the dining.
12
PETS
People allergic to pets should not
have them in the house.
At a minimum, do not allow pets in
the bedroom.
13
Molds – Fungus
Eliminating molds may help control asthma exacerbations.
14
Diagnosis of Asthma
History and patterns of symptoms
Physical examination
Measurements of lung function
– Peak flow meter
– Spirometry
15
Patient History
Recurrent attacks or episodes of wheezing?
Troublesome cough, worse particularly at night
Cough after physical activity (e.g. playing)?
H/o seasonal attacks of breathing problems.
16
Main Symptom Clues
Do the patient’s colds ‘go to the chest’ or take more
than 10 days to resolve?
Does the patient use any medication ? Is there
(relief) ? (e.g. bronchodilator) when symptoms occur
If the patient answers “YES” to any of the above
questions, suspect asthma.
Remember, the commonest cause of persistent
cough is asthma
17
Physical Examination
Wheeze
Usually heard without a stethoscope
Dyspnea
Rhonchi heard with a stethoscope
Use of accessory muscles
Remember
Absence of symptoms at the time of examination
does not exclude the diagnosis of asthma
18
Physical Examination
Hyper-expansion of the thorax
Increased nasal secretions or nasal
polyps
Atopic dermatitis, eczema, or other
allergic skin conditions
19
Screening Test – Peak Flow
Diagnosis of asthma can be suspected
by demonstrating the presence of airway
obstruction using Peak flow meter.
Peak Flow Meter is a
basic tool in a GPs office
20
Diagnostic Test – The PFT
Diagnosis of asthma can be confirmed by demonstrating the
presence of reversible airway obstruction using Spirometry.
21
Spirometry Results
FVC
Forced Vital Capacity
FEV1
Forced Expiratory Volume
in the first second
FEV1÷FVC
Ratio of the above two
PEFR
Peak Expiratory Flow Rate
FET
Forced Expiratory Time
22
Spirometry Normal Values
1.
There are no fixed ‘Normal’ values
2.
Dependent on age, sex, ht, wt, ethnicity
3.
Observed value expressed as predicted value %
FVC
Normal if > 80% of predicted
FEV1
Normal if > 80% of predicted
FEV1/FVC
At least 75%
PEFR
Normal if > 80% of predicted
FET
Less than 4 seconds
23
Typical FEV1 Tracings
Volume
FEV1
Normal Subject
> 80%
Asthmatic (After Bronchodilator)
60%
Asthmatic (Before Bronchodilator)
40%
Each FEV1 curve represents
the best of three repeat efforts
1
2 3 4
Time (sec)
5
24
Obstructive v/s Restrictive
Parameter
Normal
Obstructive
Restrictive
Problem
‘Air out’ and
‘Air in’ normal
Unable to
get ‘Air out’
Unable to
get ‘Air in’
FVC
80 % of pred
Normal or ↓
↓,↓TLC
FEV1
80 % of pred
↓-80% or less
Normal
FEV1 ÷ FVC
Min. of 75%
↓-70% or less
Normal or ↑
PEFR
80 % of pred
↓-80% or less
Normal
FET in sec
Less than 4
Prolonged > 4
Normal - < 4
25
Goals In Asthma Control
Achieve and maintain control of symptoms
Prevent asthma episodes or attacks
Minimal use of reliever medication
No emergency visits to doctors or hospitals
Maintain normal activity levels, including exercise
Maintain PF as close to normal as possible
Minimal (or no) side effects from medicine
27
Tool Kit We Have
Relievers (Quick)
Controllers (long term)
Peak Flow meter
Spirometry
Patient education
28
Asthma Treatment Today
We can completely control symptoms
Make their life as normal as possible
Treatable by general practice physicians
We do not need to be Chest Specialists!
29
It is a Dual Problem
1.
Bronchial inflammation – perpetual
1. Allergic inflammation and edema
2. Inflammatory mediators – perpetuate
3. edema and excite bronchospasm
4. Bronchial hyper reactivity to triggers
2.
Bronchospasm – acute attacks
Needs two different types of medicines
Relievers & Controllers
30
Certain Abbreviations
ICS
IBD
SABA
LABA
LTA
OCS
SR
Ach B
Inhaled corticosteroids
Inhaled bronchodilators
Short acting β agonists
Long acting β agonists
Leukotrine antagonists
Oral corticosteroids
Sustained release
Acetylcholine blockers
31
What Are Relievers?
Spasm needs reliever
– Bronchodilator drugs
– Rescue medications
– Quick relief of symptoms
– Used during acute attacks
– Action lasts for 4-6 hrs
– Not for regular use at all
32
Relievers
Rapid-acting inhaled β2-agonists
– Salbutamol, Levo Salbutamol
Anti-cholinergics
– Ipatropium, Tiotropium
Short-acting oral β2-agonists
– Salbutamol, Levo Salbutamol, Terbutaline
Systemic glucocorticosteroids (Status Asthmaticus)
Theophylline (oral) – (evidence C)
33
What Are Controllers ?
Prevent future attacks
– Reduce allergic inflammation
– Reduce inflammatory mediators
– Reduce hyper-responsiveness
– Long term control of asthma
– Prevent airway remodeling
– For regular use – well or ill
34
Let Us Question
Are we giving the right drug?
Are we giving the drug in right form?
Are we using the correct technique?
35
The Story Of Asthma Treatment
Normal
Inflamed (untreated)
Regular
Inhaled
Steroid
Remodeled
Partly
Treated
36
Most Important
All Asthma drugs should ideally be
taken through the inhaled route.
37
What Changes Their Life ?
ICS
Inhaled corticosteroids
ICS are the most potent and effective antiinflammatory medication currently
available for Asthma *
*GINA (NHLBI & WHO Workshop Report)
*Guidelines for the diagnosis and management of Asthma NIH, NHLBI
38
Let Us Believe First
Corticosteroids ??
Inhaled medicines ?? Patients’ wrong belief
Parents / Grand parents
Neighbors / ‘friends’
First of all, let us believe in science
Let us explain and convince them
Let us change their lives – to happy lives
39
Let Us Unlearn
Adrenaline s/c, thank heavens we forgot !!
Deriphyllin + Betnesol I.V - give up please - Must !!
Oral SABA and LABA – Restrict their use !!
Theophylline in any form beware !!
Systemic steroids – Not at all the choice !!
ICS and IBD are the Rx.
40
Remember
Instead of asthma
controlling our patient,
allow our patient to
control his / her asthma
41
Why Inhalation Treatment
Oral
Inhaled route
Slow onset of action
Rapid onset of action
Large dosage used
Less amount of drug
Greater side effects
Drug delivered to the site
Erratic absorption
Better tolerated
Not useful in acute
illness
Treatment of choice
in acute symptoms
42
Preventers
Inhaled corticosteroids
Budesonide/ beclomethasone/ fluticasone – use any
Start (400-1000 mcg/day approx. in 2 divided doses)
Maintain for 3 months
Taper slowly and keep at 200 mcg
Safe for long-term use (years)
43
ICS – How safe are they?
They are very safe
Even in small children for several years
30% of Olympic athletes use ICS
Not anabolic (performance-enhancing) steroid
Even highest ICS dose is safer than low dose
oral steroid or beta agonist
Best “Addiction” for asthmatics
44
ICS are safe even for a child
400 mcg/day (budesonide)
Over 9 years of continuous use
No growth retardation
Uncontrolled asthma causes growth retardation
Pedersen & Agertoft NEJM 2000
45
Not All Are Same !!
Beclomethasone 6 hrly + Salbutamol 6th hrly
Budesonide 12 hrly + Salmeterol 12 hrly
Salmeterol 12 hrly + Ipatropium 12 hrly
Fluticasone 24 hrly + Formoterol 24 hrly
Formoterol 24 hrly + Tiotropium 24 hrly
Choice is based on
1. If need is urgent and uncontrolled – 6 hrly
2. If need is maintenance, well contr. – 12 hrly
3. If stabilized and wants convenience – 24 hrly
46
Pregnancy and Asthma
Don’t x-ray (if possible)
All asthma medication is safe
Even oral corticosteroids are safe for exacerbations
Uncontrolled asthma during pregnancy is a serious
risk factor for foetal distress and anoxia
Thorax Supplement
47
Leukotrine Modifiers
Oral Leukotrine antagonist – anti inflammatory
Not as effective as inhaled steroid
May be first-line for 2 to 5 yr. olds.
Montelukast available; Zafirlukast is not in India
4 mg, 5 mg, 8 mg tabs available
Can be add on to ICS, IBD inhalers
48
Step Up and Down – Acute Asthma
SABA (IBD) in full doses
SABA Increase frequency or Nebulize
SABA as above + IPA (IBD), then add
OCS (Methyl prednisolone) 30-60 mg for 3 to 10 days - add
ICS (1000 mcg) / day and maintain for 6 weeks minimum
Gradually bring down doses and maintain with ICS
If symptoms are not relieved – Check the technique compliance
Look for aggravating factors like
– GE Reflux, Emotions/ Stress, Sinusitis, Allergic Rhinitis
? Role for Theophylline; Oral SABA or LABA not very useful
49
The Step Care Approach - Prevent
ICS
ICS + LABA (IBD)
ICS + LABA (IBD) + Double Dose ICS
ICS (DD) + LABA + LTA (oral)
ICS (DD) + LABA + LTA + OCS
ICS (DD) + LABA + LTA + OCS + TIO (IBD)
SR Theophylline may be an add on
SABA or LABA Oral + IPA (IBD) may be a useful add on
No long acting steroid injections
No injectable or short acting Theophylline
50
Controlled
REDUCE
LEVEL OF CONTROL
THERAPEUTIC ACTION
Maintain and find lowest
controlling step
Consider stepping up
to gain control
Uncontrolled
Exacerbation
INCREASE
Partly controlled
Step up until controlled
Treat as exacerbation
REDUCE
STEP
1
INCREASE
TREATMENT STEPS
STEP
STEP
STEP
2
3
4
STEP
5
51
52
Why doctors don’t use inhalation Rx ?
Status quo – No mood to unlearn
“My practice is good or ‘great’
Oral therapy is easy
Too busy
Difficulty in convincing
Cost (in fact, in the long run economical)
Headache to explain
53
Drug Delivery Options
Metered dose inhalers (MDI)
Dry powder inhalers (Rota haler)
Dry powder compressed for Disc haler
Spacers / Holding chambers
Nebulizers
54
Demonstration of the correct technique
Ask the patient to demonstrate
to you the technique
55
Drug Delivery - Options
1. Dexterity
pMDI – Metered Dose Inhalers
2. Hand grip strength
Rota halers, Disk halers
3. Co-ordination
Space halers
4. Severity of ROAD
Zerostats
5. Educational level
Nebulizers
6. Age of the patient
Oxygen mixed delivery
Oral tablets, syrups
Parenteral – I.M or I.V use
7. Ability to inhale and
synchronize
56
What Drug Delivery Method ?
Very young or very old
MDI + LV Spacer
Elderly
MDI + SV spacer
Young children > 7 yrs
DPI (Rota haler)
Adults - educated
MDI alone
Adults - no co-ordination
DPI (Rota haler)
Clinic setting
MDI + Spacer
Clinic - emergency
Nebulizer
Choice is to be individualized; Trial and error
may be needed; Cost may be a factor
57
Inhalation Devices
Rotahaler
Dry powder Inhaler
Metered dose
inhaler or MDI
Spacer
Space halers
58
MDI + Large Volume Spacer
59
The Zerostat Advantage
1.
Non-static spacer made up of polyamide material
2.
Increased respirable fraction; Increased deposition of
drug in the airways
3.
Increased aerosol half-life; Plenty of time for the patient
to inhale after actuation of the drug
4.
No valve; No dead space; Less wastage of the drug
5.
Small, portable, easy to carry, child friendly
60
Disk haler – Nebulizer
61
Nebulizer Therapy
1.
Severe breathlessness despite using inhalers
2.
Assessment should be done for improvement
3.
Choice between a facemask or mouth piece
4.
Equipment servicing and support are essential
5.
0.5 ml of Ipa + 0.5 ml of Sal + 5 ml of Nacl (not DW)
6.
If decided to use ICS (FEV1 < 50%) - 0.5 ml of Buduso.
7.
15 minutes and slow or moderate flow rate
8.
Can be repeated 2 to 3 times a day – Mouth Wash
62
Patient Education
Explain nature of the disease (inflammation)
Explain action of prescribed drugs
Stress the need for regular, long-term therapy
That way only we can convince
Allay fears and concerns
Peak flow testing
Symptom, treatment diary
63
Patient Education
Asthma is a common disorder
It can happen to anybody, May not be life long
It is not caused by supernatural forces
Asthma is not contagious, All kin needn’t be affected
Recurrent attacks of cough with or without wheeze
Between attacks people with asthma lead normal lives
In most cases, there is some family history of allergy
64
Patient Education
Can be effectively controlled, although can’t be cured.
Effective asthma management programs include
education, objective measures of lung function,
environmental control, and pharmacologic therapy.
A stepwise approach to pharmacologic therapy is
recommended. The aim is to accomplish the goals of
therapy with the least possible medication.
65
Yours Faithfully Urges
A little time spent talking to our patients –
really is a great investment.
This may make all the difference between
a happy life and pulmonary invalidity
66
Life Time Happiness
Can we dare to make
them pulmonary invalids ?
Let Us Give Them
Life Time Happiness
68