BRONCHIAL ASTHMA
advertisement
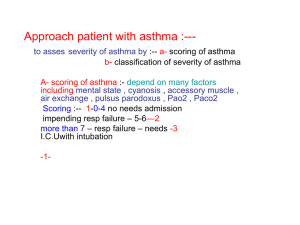
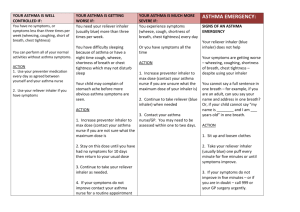
BRONCHIAL ASTHMAMANAGEMENT ABIRAMI SA DEFINITION A chronic inflammatory disorder of the airway (Airway hyper responsiveness) Infiltration of mast cells, eosinophils and lymphocytes Widespread, variable and often reversible airflow limitation Diagnosis Symptoms: cough, wheeze, dyspnea Investigations: 1. PFT 2. Chest Xray 3. AEC RED FLAG SIGNS 1. RR is increased 2. DANGER SIGNS: drowsiness, agitation, cyanosis, inability to vocalise, silent chest 3. DEHYDRATION 4. PNEUMOTHORAX 5. HYPOTENSION 6. DIAPHORESIS 7. PULSUS PARADOXUS 8. PARADOXICAL RESPIRATION 9. CHEST INDRAWING ACUTE SEVERE ASTHMA CLINICAL FEATURES ALERT, NORMAL TONE INCREASED RR, HR, BREATH SOUNDS NORMAL PERFUSION PEFR < 60% SPO2 < 90% TREATMENT 1. O2 by mask 2. Neb. with Salbutamol [0.03ml/kg/dose] + Oral Prednisolone [1mg/kg/day] If improving, continue neb. Q4h/q6h & discharge with Oral Salb & steroids x 3-4 days If not improving treat as life threatening asthma LIFE THREATENING ASTHMA CLINICAL FEATURES Agitated / irritable / inconsolable Increased RR, HR Decreased breath sounds Reduced perfusion Spo2 < 92% Danger signs + TREATMENT 1. O2 by mask 2. investigations: CBC, electrolytes, CXR, ABG at later stage 3. Start antibiotics: Ampicillin [100mg/kg/day] 4. IVF as maintainance 5. Triple nebulisation: Salb [0.03ml/kg/dose] Budesonide [0.5mg/kg/dose] Ipratropium [0.5 ml < 10 kg, 1 ml > 10 kg] 6. IV Hydrocortisone 10 mg/kg 7. If improving, continue neb. with Salb 1-3 hrly + Ipravent q6h, and discharge with oral steroids, antibiotics & salb 8. If no improvement, start IV Aminophylline [5 mg/kg] loading dose in 20 ml dextrose solution followed by infusion Aminophylline [1mg/kg/hr] + Hydrocortisone [1mg/kg/hr] 9. Start IV MgSO4 0.1 ml/kg 50% solution in 50 ml NS given as IV over 30 min (q6h) 10. Methyl prednisolone 2 mg/kg bolus followed by 1 mg/kg/dose q8h simultaneously 11. If no improvement, TERBUTALINE 10 mg/kg IV bolus over 10 min and then 210 mg/kg/hr as IV 12. If still no improvement, consider MECHANICAL VENTILATION INDICATIONS FOR MECH. VENTILATION Exhausted/ Comatose child Silent chest ABG: PO2 <60mmhg, PCO2 >60 mmhg LONG TERM MANAGEMENT OF ASTHMA Classification of Asthma Severity CLASSIFY SEVERITY STEP 4 Severe Persistent Clinical Features Before Treatment Nighttime PEF Day Symptoms Symptoms Continuous <60% predicted Frequent Limited physical Variability >30% activity STEP 3 Moderate Persistent Daily Use b2-agonist daily Attacks affect activity >1 time a week STEP 2 Mild Persistent >1 time a week but <1 time a day >2 times a month < 1 time a week Asymptomatic and normal PEF between attacks <2 times a month STEP 1 Intermittent >60%-<80% predicted Variability >30% >80% predicted Variability 2030% >80% predicted Variability <20% The presence of one of the features of severity is sufficient to place a patient in that category. Global Initiative for Asthma (GINA) WHO/NHLBI, 2002 CATEGORY DAILY MANAGEMENT STEP 1 No daily medications STEP 2 Inhaled SABA + Inhaled low dose CS [<400mcg] / Cromolyn / SR / LTRA STEP 3 Inhaled SABA + Inhaled low – med dose CS [400-800mcg] + Inhaled LABA / SR Theophylline STEP 4 Inhaled SABA + Inhaled high dose CS [400 – 1000mcg] + Inhaled LABA / SR Theophylline + low dose CS on alt. days BRONCHODILATORS SALBUTAMOL INHALER 100 mcg: 1 or 2 puffs as necessary LEVOSALBUTAMOL INHALER 50 mcg : 1 or 2 puffs as necessary Long acting b2 agonists: Bambuterol, Formoterol Salmeterol OTHERS Corticosteroids Prednisolone, Betamethasone Beclomethasone, Budesonide Fluticasone Anti-leukotrienes Montelukast, Zafirlukast Xanthines Theophylline SR Mast cell stabilisers Sodium cromoglycate COMBINATIONS Salmeterol/Fluticasone Formoterol/Budesonide Salbutamol/Beclomethasone All Asthma Drugs Should Ideally Be Taken Through The Inhaled Route Why inhalation therapy? Oral Slow onset of action Large dosage used Greater side effects Not useful in acute symptoms Inhaled route Rapid onset of action Less amount of drug used Better tolerated Treatment of choice in acute symptoms Aerosol delivery systems Commonly used Metered dose inhalers Dry powder inhalers (Rotahaler) Spacers / Holding chambers Inhalation devices you can use Dry Powder Inhaler Metered Dose inhaler Spacer Advantages of Spacer No co-ordination required No cold - freon effect Reduced oropharyngeal deposition Increased drug deposition in the lungs Small, portable, easy to carry Child friendly Rotahaler - The dry powder advantage Overcomes hand-lung coordination problems that are encountered with MDIs. Can be easily used by children. Can take multiple inhalations if the entire drug has not been inhaled in one inhalation. Age-wise selection of inhaler devices < 3 years – MDI + Spacer + Mask or nebulisers 3 – 5 years – MDI + Spacer + Mask or Rotahaler 5 – 8 years – Rotahaler or MDI + Spacer > 8 years – Rotahaler or MDI + Spacer Goals to Be Achieved in Asthma Control Achieve and maintain control of symptoms Prevent asthma episodes or attacks Minimal use of medication No emergency visits to doctors or hospitals Maintain normal activity levels, including exercise Maintain pulmonary function as close to normal as possible Minimal (or no) adverse effects from medicine Patient Education Explain nature of the disease (i.e. inflammation) Stress need for regular, long-term therapy Allay fears and concerns Key Messages Asthma can be effectively controlled, although it cannot be cured. Effective asthma management include education, objective measures of lung function, environmental control, and pharmacologic therapy. Thank you