Click to British Guidelines on the Management of Asthma
advertisement

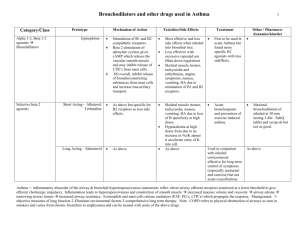
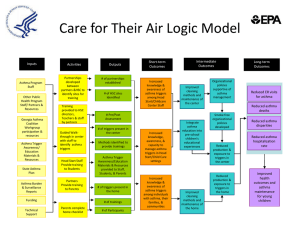
British Guideline on the Management of Asthma Aims • Review of current SIGN/BTS guidelines – Diagnosing Asthma – Stepwise management of Asthma – Managing Acute Asthma – When to admit Age Groups • Children • Adults Diagnostic Algorithms • Clinical features – Increase/decrease the probability of Asthma • Diagnostic probability – Low, intermediate and high. Clinical features & Probability • Increase – Wheeze, cough, shortness of breath, tight chest. – Worse at night/morning – Triggers • Exercise,allergen,cold air, drugs – – – – – Atopy FH asthma/atopy Widespread wheeze Response to treatment Unexplained low FEV1 or eosinophilia • Decrease – – – – – – – – – – No interval symptoms Cough only Moist cough Hyperventilation symptom Normal examination Normal PF/spirometry No response to Rx Cardiac disease Voice disturbance Significant smoking history Management • Non-pharmacological – Breast feeding – Avoidance of tobacco smoke – Weight reduction • Pharmacological Pharmacological Management • Aim for complete control – No daytime symptoms, no night time awakening, no need for rescue meds, no exacerbations, normal activity, normal lung function. • Stepwise approach – Start at most appropriate step – Early control – Maintain by stepping up or down Stepwise Management in Adults Management in Children 5-12 yrs Management in Children <5 yrs Management of Acute Asthma Management of Acute Asthma • Assessment – Clinical features – PEF – Pulse oximetry – Blood gases (ABG) – Chest X-ray • Not routine – Suspected pneumothorax, consolidation, life threatening, failure to respond, requiring ventilation Management of Acute Asthma • Moderate – PEFR >50-75% – No severe features • Severe – – – – PEFR 33-50% RR ≥ 25 (adult), >30 (>5yrs), >40 (2-5yrs) HR ≥ 110 (adult), >125 (>5yrs), >140 (2-5yrs) Unable to complete sentences or feed • Life threatening – PEFR <33% – SpO2 <92% – Silent chest, cyanosis, exhaustion, altered consciousness Management of Acute Asthma • Oxygen – Hypoxic patients – aim 94-98% – Drive nebulisers with oxygen • 2 agonist bronchodilators – As early as possible – Consider continuous nebulisers if poor initial response • Oral steroids • Ipratropium bromide • IV magnesium sulphate – Poor response to 2 agonist or life threatening • IV salbutamol/aminophylline - Paediatrics Admission criteria - Adults • Life threatening – Immediately • Severe – If any features of severe attack after initial treatment Admission criteria - Children • Severe of life threatening – Immediately • Moderate – No improvement after 10 puffs of 2 agonist Difficult Asthma • Persistent symptoms or frequent exacerbations despite step 4 or 5 – Confirm diagnosis – Consider poor compliance – Consider psychosocial assessment Conclusion • Asthma is frequently under treated • Use current guidelines to aid diagnosis and help in acute and chronic management • If patients are not responding as you would expect – Is the diagnosis right? – Are they taking the appropriate medication? – Are psychological or social factors hindering management?