Asthma: Definition, Causes, Diagnosis & Treatment Guide
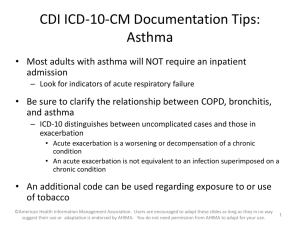
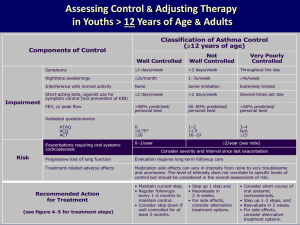
advertisement
Asthma is a condition characterized by paroxysmal narrowing of the bronchial airways due to inflammation of the bronchi and contraction of the bronchial smooth muscle. The inflammatory component is central to the pathogenesis of symptoms: dyspnea, cough, and wheezing. Common causes of acute asthma include viral upper respiratory infections; exposure to allergens (eg, dustmites, animal dander); smoke inhalation; and cold, dry weather Incidence of acute asthma, defined as the number of persons who develop asthma within a specific time period, is approximately 0.2-0.4% annually. Childhood asthma persists into adulthood in approximately 50% of cases. Those with symptoms persisting into the second decade of life usually have asthma throughout adulthood. Asthma prevalence is 6-10% (ie, 20-25 million persons); one half of these cases are children (ie, 8-20% of all children). Overall, acute asthma represents about 2% of all ED visits Mild intermittent asthma Symptoms of cough, wheeze, chest tightness, or difficulty breathing less than twice a week Flare-ups brief, but intensity may vary Nighttime symptoms less than twice a month No symptoms between flare-ups Lung function test FEV1 equal to or above 80% of normal values Peak flow less than 20% variability am-to-am or am-to-pm, day-to-day. Mild persistent asthma Symptoms of cough, wheeze, chest tightness, or difficulty breathing 3-6 times a week Flare-ups may affect activity level Nighttime symptoms 3-4 times a month Lung function test FEV1 equal to or above 80% of normal values Peak flow less than 20-30% variability Moderate persistent asthma Symptoms of cough, wheeze, chest tightness, or difficulty breathing daily Flare-ups may affect activity level Nighttime symptoms 5 or more times a month Lung function test FEV1 above 60% but below 80% of normal values Peak flow more than 30% variability Differential Diagnoses Chronic Obstructive Pulmonary Disease and Emphysema Anaphylaxis (adult, pediatric) Bronchiolitis (pediatric) Foreign body ingestion (pediatric, adult incompetent, neurologically impaired) Polyarteritis nodosa Adrenal insufficiency if steroids stopped too abruptly Congestive heart failure and myocarditis Pulmonary embolism (especially multiple) Upper airway disease Panic disorder and hyperventilation syndrome Pneumonia, bronchitis Paradoxic vocal cord dysfunction F I G U R E 5 – 1 . CLASSIFYING SEVERITY O F ASTHMA EXACERBATIONS I N THE URGENT OR EMERGENCY CARE SETTING Note: Patients are instructed to use quick-relief medications if symptoms occur or if PEF drops below 80 percent predicted or personal best. If PEF is 50–79 percent, the patient should monitor response to quick-relief medication carefully and consider contacting a clinician. If PEF is below 50 percent, immediate medical care is usually required. In the urgent or emergency care setting, the following parameters describe the severity and likely clinical course of Symptoms and Signs Initial PEF (or FEV1) Clinical Course Mild Dyspnea only with activity (assess tachypnea in young children) PEF ≥70 percent predicted or personal best Usually cared for at home Prompt relief with inhaled SABA Possible short course of oral systemic corticosteroids Key: ED, emergency department; FEV1, forced expiratory volume in 1 second; ICU, intensive care unit; PEF, peak expiratory flow; SABA, short-acting beta2-agonist Moderate Dyspnea interferes with or limits usual activity PEF 40−69 percent predicted or personal best Usually requires office or ED visit Relief from frequent inhaled SABA Oral systemic corticosteroids; some symptoms last for 1–2 days after treatment is begun Key: SABA, short-acting beta2-agonist Severe Dyspnea at rest; interferes with conversation PEF <40 percent predicted or personal best Usually requires ED visit and likely hospitalization Partial relief from frequent inhaled SABA Oral systemic corticosteroids; some symptoms last for >3 days after treatment is begun Adjunctive therapies are helpful Subset: Life threatening Too dyspneic to speak; perspiring PEF <25 percent predicted or personal best Requires ED/hospitalization; possible ICU Minimal or no relief from frequent inhaled SABA Intravenous corticosteroids Adjunctive therapies are helpful Key: ED, emergency department; ICU, intensive care unit; PEF, peak expiratory flow; SABA, short-acting beta2-agonist Inhaled Short-Acting Beta2-Agonists (SABA) Albuterol Nebulizer solution (0.63 mg/3 mL,1.25 mg/3 mL,2.5 mg/3 mL,5.0 mg/mL) 0.15 mg/kg (minimum dose 2.5 mg) every four hours as needed Status Asthmaticus; in ED, may give every 20 minutes for 3 doses then 0.15–0.3 mg/kg up to 10 mg every 1–4 hours as needed, or 0.5 mg/kg/hour by continuous nebulization. May mix with ipratropium nebulizer solution. Ipratropium bromide Nebulizer solution (0.25 mg/mL) 0.25–0.5 mg every 20 minutes to four hours May mix in same nebulizer with albuterol. Should not be used as first-line therapy; should be added to SABA therapy for severe exacerbations. Ipratropium has not been shown to provide further benefit once admitted to hospital MDI (metered dose inhaler) (90 mcg/puff) 2 puffs every 4 hours as needed Status Asthmaticus; In ED, 4–8 puffs every 20 minutes for 3 doses, then every 1–4 hours inhalation maneuver as needed. Add mask in children <4 years. 4–8 puffs every 20 minutes up to 4 hours, then every 1–4 hours as needed. Asthma Exacerbation • Add steroid if not improving with inhaled albuterol/salbutamol • Prednisone 1-2mg/kg/day daily or divided BID • If severe or cannot take po; use IV; • Methylprednisolone 2-4mg/kg/day divided BID or QID Asthma Exacerbation • Other medicines used less often include; • subcutaneous epinephrine IV magnesium theophylline