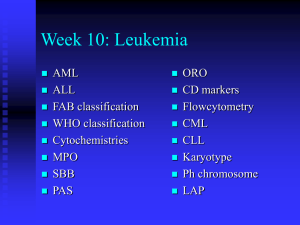
Document
advertisement
Leukemia/Lymphoma Components and General Properties of Blood Seven kinds of formed elements Erythrocytes: red blood cells (RBCs) Platelets (thrombocytes) (clotting cells) Cell fragments from special cell in bone marrow Leukocytes: white blood cells (WBCs)-5 kinds 18-2 Components and General Properties of Blood Five leukocyte types divided into two categories Granulocytes (with granules) • 3)Neutrophils • 4)Eosinophils • 5)Basophils Agranulocytes (without granules) • 6)Lymphocytes • 7)Monocytes Components and General Properties of Blood Monocyyte Small lymphocyte Platelets Neutrophil Eosinophil Small lymphocyte Erythrocyte Young (band) neutrophil Neutrophil Monocyte Large lymphocyte Neutrophil Basophil Leukocytes Least abundant formed element – 5,000 to 10,000 WBCs/L Protect against infectious microorganisms and other pathogens Conspicuous nucleus Spend only a few hours in the bloodstream before migrating to connective tissue Retain their organelles for protein synthesis Granules All WBCs have lysosomes called nonspecific (azurophilic) granules: inconspicuous so cytoplasm looks clear Granulocytes have specific granules that contain enzymes and other chemicals employed in defense against pathogens 18-5 Types of Leukocytes Granulocytes Neutrophils (60% to 70%): polymorphonuclear leukocytes Barely visible granules in cytoplasm; three- to five-lobed nucleus Eosinophils (2% to 4%) Large red-orange granules; Basophils (less than 1%) Large, abundant, violet granules 18-6 Agranulocytes Lymphocytes (25% to 33%) Variable amounts of bluish cytoplasm (scanty to abundant); ovoid/round, uniform dark violet nucleus Monocytes (3% to 8%) Largest WBC; generally ovoid, kidney-, or horseshoe-shaped nucleus Granulocytes Neutrophils—increased numbers in bacterial infections Phagocytosis of bacteria Release antimicrobial chemicals Eosinophils—increased numbers in parasitic infections, collagen diseases, allergies, diseases of spleen and CNS Phagocytosis of antigen–antibody complexes, allergens, and inflammatory chemicals Release enzymes to destroy large parasites 18-8 Basophils—increased numbers in chickenpox, sinusitis, diabetes Secrete histamine (vasodilator): speeds flow of blood to an injured area Secrete heparin (anticoagulant): promotes the mobility of other WBCs in the area Agranulocytes Lymphocytes—increased numbers in diverse infections and immune responses Destroy cells (cancer, foreign, and virally infected cells) “Present” antigens to activate other immune cells Coordinate actions of other immune cells Secrete antibodies and provide immune memory 18-10 Agranulocytes Monocytes—increased numbers in viral infections and inflammation Leave bloodstream and transform into macrophages Phagocytize pathogens and debris “Present” antigens to activate other immune cells—antigenpresenting cells (APCs) 18-11 The Leukocyte Life Cycle Leukopoiesis—production of white blood cells Pluripotent stem cells (PPSCs) Myeloblasts—form neutrophils, eosinophils, basophils Monoblasts—form monocytes Lymphoblasts give rise to all forms of lymphocytes 18-12 Leukopoiesis Pluripotent stem cell Colony-forming units (CFUs) Mature cells Precursor cells Eosinophilic myeloblast Eosinophilic promyelocyte Eosinophilic myelocyte Eosinophil Basophilic CFU Basophilic myeloblast Basophilic promyelocyte Basophilic myelocyte Basophil Neutrophilic CFU Neutrophilic myeloblast Neutrophilic promyelocyte Neutrophilic myelocyte Neutrophil Monocytic CFU Monoblast Promonocyte B prolymphocyte Lymphocytic CFU 18-13 leaves Eosinophilic CFU Lymphoblast Monocyte B lymphocyte T prolymphocyte T lymphocyte NK prolymphocyte NK cell What Is Leukemia? Cancer of the white blood cells Acute or Chronic Affects ability to produce normal blood cells Bone marrow makes abnormally large number of immature white blood cells called blasts History Means “white blood” in Greek Discovered by Dr. Alfred Velpeau in France, 1827 Named by pathologist Rudolf Virchow in Germany, 1845 Leukocyte Disorders Leukemia—cancer of hemopoietic tissue that usually produces an extraordinary high number of circulating leukocytes and their precursors Myeloid leukemia: uncontrolled granulocyte production Lymphoid leukemia: uncontrolled lymphocyte or monocyte production 18-16 Acute vs Chronic Leukemia Acute leukemia: appears suddenly, progresses rapidly, death within months –blasts found in peripheral blood Chronic leukemia: undetected for months, survival time average of 3 years Effects: normal cell percentages disrupted; impaired clotting; opportunistic infections Main Types Acute Lymphocytic Leukemia (ALL) Acute Myelogenous Leukemia (AML) Chronic Lymphocytic Leukemia (CLL) Chronic Myelogenous Leukemia (CML) Demographics of Leukemia Patients (2001 Data) CLL=Chronic Lymphocytic ALL=Acute Lymphocytic ALL 11% others 17% CML=Chronic Mylogenous AML=Acute Mylogenous CML 15% CLL 26% AML 31% Total Reported Cases = 31,500 Pictures Of Blood Platelet White Cell Platelet Red Cell Red Cell Blasts White Cell Normal human blood Blood with leukemia Development of Leukemia in the Bloodstream Stage 1- Normal Stage 2- Symptoms Stage 3- Diagnosis Legend White Cell Red Cell Platelet Blast Germ Stage 5a- Anemia Stage 4- Worsening Stage 5b- Infection Causes High level radiation/toxin exposure Viruses Genes Chemicals Mostly unknown Signs and Symptoms of AML Insidious nonspecific onset Pallor due to anemia Febrile (fever) due to ineffective WBC Petechiae (skin bruising) due to thrombocytopenia Bone pain Petechiae Typical Labs of AML Leukocytosis Blastemia Leukemic hiatus Auer rods – only found in myelocytic blasts Thrombocytopenia Anemia >20% blasts in Bone Marrow Auer Rods Auer Rod CD Markers The cluster of differentiation (cluster of designation) (often abbreviated as CD) is a protocol used for the identification and investigation of cell surface molecules providing targets for immunophenotyping of cells. The CD markers can be used to identify the type of cell. Other Findings CD 13 and CD 33 in flowcytometry Cytochemistries-stains that can be used to differentiate leukemias Myeloperoxidase Sudan black B Choloroacetate esterase (specific) Nonspecific esterase Flow Cytometry Large clustering of CD 33s shows presence of blasts FAB (1976) Classification M0 -- Undifferentiated AML M1 -- AML without maturation M2 -- AML with maturation M3 -- Acute Promyelocytic Leukemia M4 -- Acute Myelomonocytic Leukemia M5 -- Acute Monocytic Leukemia M6 -- Erythroleukemia (DiGuglielmo’s) M7 -- Megakaryoblastic Leukemia Myeloperoxidase (MPO) p-Phenylene diamine + Catecol + H2O2 MPO > Brown black deposits Brown deposits considered to be a positive testdifferentiates AML from other leukemias M1 and M2 M3 M4 M5 Chloracetate (Specific) Esterase Myeloid Cell Line Naphthol-ASD-chloracetate CAE > Free naphthol compounds + Stable diazonium salt (eg, Fast Corinth) > Red deposit Non-Specific Esterase Monocytic Line Naphthyl acetate ANAE > Free naphthyl compounds +Stable diazonium salt (eg, Fast blue RR) > Brown deposits FAB vs WHO Classifications of Hematologic Neoplasm FAB criteria Morphology Cytochemistry WHO criteria Morphology Immunophenotyping Genetic features Karyotyping Molecular testing Clinical features WHO Classification of AML AML with recurrent cytogenic translocations AML with multi-lineage dysplasia AML and myelodysplasia, therapy related AML, not otherwise categorized AML with Recurrent Cytogenetic Translocations (WHO 1995) t(8;21) -- some maturation of neutrophilic line; rare in older patients; AML1/ETO fusion protein; >90% FAB M2 t(15;17) -- APL (granular and microgranular variants); retinoic acid receptor (RAR) leukemias; middle aged adults; DIC inv(16) or t(16;16) -- monocytic and granulocytic; abnormal eosinophilic component 11q23 -- monocytic; children; most common is t(9;11) Lymphocytic Leukemias Can involve T or B lymphocytes B lymphs mature in bone marrow Responsible for making antibodies T lymphs go to thymus to mature Are cytotoxic cells of immune system FAB Classification of ALL L1: Small homogeneous blasts; mostly in children L2: Large heterogeneous blasts; mostly in adults L3: “Burkitt” large basophilic B-cell blasts with vacuoles L2 L3 Periodic Acid Schiff Periodic acid + Glycogen oxidation > Aldehyde + Schiff reagent (para-rosaniline, Na metabisulfite) > Red deposit ALL Cytochemistries Oil Red O: stains L3 vacuoles Terminal deoxynucleotidyl transferase (Tdt): DNA polymerase in early lymphoblasts Cell surface markers (CD’s) Cytoplasmic and surface immunoglobulins: B-cell line T-cell receptor (TCR) WHO Classification of Lymphoproliferative Syndromes Precursor B Lymphoblastic Leukemia/Lymphoma (ALL/LBL) -- ALL in children (80-85% of childhood ALL); LBL in young adults and rare; FAB L1 or L2 blast morphology Precursor T ALL/LBL -- 15% of childhood ALL and 25% of adult ALL Burkitt Leukemia/Lymphoma (FAB L3) Prognosis Indicators Favorable Poor WBC < 50,000/L 50,000/L Age 1 - 10 < 1 or 10 Gender Female Male Blast B-cell T-cell and mixed Karyotype Hyperploidy Trisomy 4, 10, 17 t(12;21) (TEL/AML1) Hypoploidy Trisomy 5 t(1;19 (E2A/PBX1) Mixed lineage leukemia T(9;22) (Ph) BM blast count Mkd reduction at day 7 during induction Mild reduction at day 7 Burkitt’s Lymphoma CML Typical Labs in CML Leukocytosis with blastemia Thrombocytosis Basophilia Micro-megakaryocytes Low LAP score (intermediate if infected) About 10% blasts in BM Philadelphia chromosome Bone marrow aspirate and biopsy Conventionally, a leukocytosis exceeding 50,000 WBC/mm3 with a significant increase in early neutrophil precursors is referred to as a leukemoid reaction. Serum leukocyte alkaline phosphatase is normal or elevated in leukemoid reaction, but is depressed in chronic myelogenous leukemia. Leukemoid reactions are generally benign and are not dangerous in and of themselves, although they are often a response to a significant disease state Historically, various clues including the leukocyte alkaline phosphatase score and the presence of basophilia were used to distinguish CML from a leukemoid reaction. However, at present the test of choice in adults to distinguish CML is an assay for the presence of the Philadelphia chromosome, either via cytogenetics and FISH, or via PCR for the BCR/ABL fusion gene. Leukocyte Alkaline Phosphatase (LAP) Naphthol AS-MX phosphate LAP at pH8.6 > Naphthol AS-MX + Diazonium salt (eg, Fast blue RR) > Insoluble pigment LAP Score Count 100 consecutive segmented neutrophils and bands Score: 0 = no granules 1+ = occasional diffuse granules 2+ = moderate number of granules 3+ = many strongly positive granules 4+ = confluent strongly positive granules 0 2+ 1+ 3+ 4+ LAP Score Example: 0 1+ 2+ 3+ 4+ x x x x x 35 cells 30 cells 20 cells 10 cells 5 cells = 0 = 30 = 40 = 30 = 20 120 LAP Score Philadelphia Chromosome 9 ;22 translocation almost specific to CML Karyotype to visualize Ph chromosome Produces BCR/c-abl fusion oncogene Gene product p190 is a hyperactive tyrosine kinase Ph chromosome seen in ALL produces p210 and chronic neutrophilic leukemia produces p230 Karyotype 46,XX,t(9;22)(q34;q11.2) -- Ph chromosome FISH showing the BCR (green), ABL (orange), and BCR-ABL fusion signals (arrow): A=positive (contains a residual ABL signal), B=normal Chronic Lymphocytic Leukemia Exclusive in elderly Lymphocytosis unrelated to viral infection Hyper-mature lymphocytes with highly condensed nuclei Smudge cells CLL PB and BM Smudge cell Bone Marrow