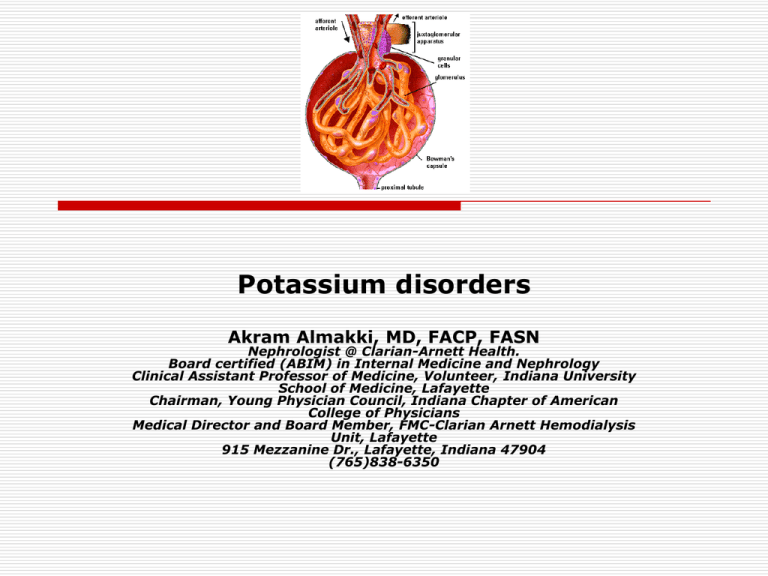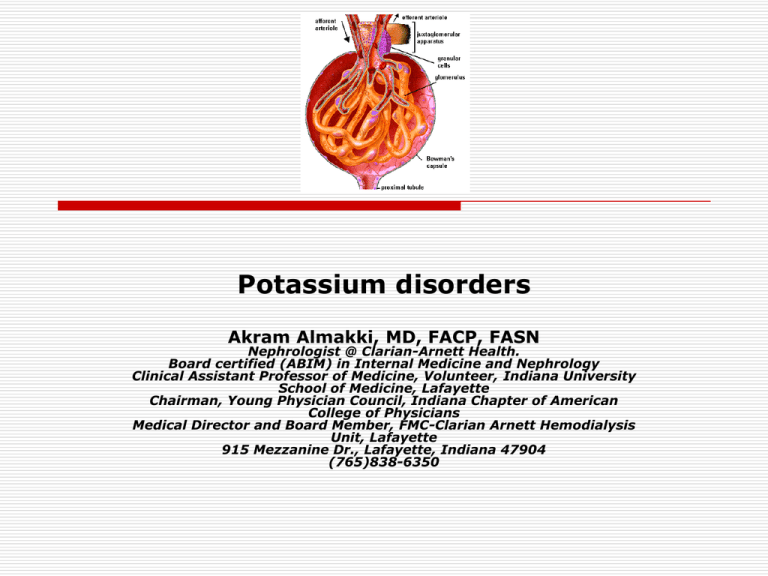
Potassium disorders
Akram Almakki, MD, FACP, FASN
Nephrologist @ Clarian-Arnett Health.
Board certified (ABIM) in Internal Medicine and Nephrology
Clinical Assistant Professor of Medicine, Volunteer, Indiana University
School of Medicine, Lafayette
Chairman, Young Physician Council, Indiana Chapter of American
College of Physicians
Medical Director and Board Member, FMC-Clarian Arnett Hemodialysis
Unit, Lafayette
915 Mezzanine Dr., Lafayette, Indiana 47904
(765)838-6350
REGULATION OF BODY
POTASSIUM
-K+ is the major intracellular ion
-Only 2% is in the ECF at a concentration of only 4 mEq/L
-K+ is taken up by all cells via the Na-K ATPase pump
-K+ is one of the most permeable ion across cell
membranes and exits the cells mostly via K channels (and
in some cells via K-H exchange or via K-Cl cotransport)
potassium homeostasis
External potassium balance is determined by rate of potassium intake
(100 meq/day) and rate of urinary (90 meq/day) and fecal excretion
(10 meq/day).
Internal potassium balance depends on distribution of potassium between
muscle, bone, liver, and red blood cells (RBC) and the extracellular fluid (ECF).
Roles of K
Major ion determining the resting membrane electrical
potential, which in turn, limits and opposes K efflux
Changes in K concentrations (particularly in the ECF)
have marked effects on cell excitability (heart, brain,
nerve,muscle).
Major intracellular osmotically active cation and
participates in cell (intracellular) volume regulation
(exits with Cl when cells swell).
Critical for enzyme activities and for cell division and
growth
Intracellular K participates in acid base regulation
through exchange for extracellular H and by
influencing the rate of renal ammonium production
Cellular K buffering
When K is added to the ECF, most of the added K is
taken up by the cells, reducing the ECF K+ increase
If K is lost from the ECF, some K+ leaves the cells,
reducing the ECF K decline
Buffering of ECF K through cell K uptake is impaired in
the absence of aldosterone or of insulin or of
catecholamines
Cell K exit to the ECF increases when osmolarity
increases (as in diabetes mellitus) and in metabolic
acidosis, when it is exchanged for ECF protons (H+)
When cells die, they release their very high K content
to the ECF
Renal regulation of Potassium
In normal function, renal K excretion balances most of the K intake
(about 1.5 mEq/Kg per day)
Proximal Tubule reabsorbs about 2/3 of the filtrate water, it also
reabsorbs about 2/3 (66%) of the filtered K (mostly passive )
Along the descending limb of the loop of Henle, K is secreted into
the tubule lumen from the interstitium
Along the thick ascending limb, K is reabsorbed via Na-K-2 Cl
cotransport
Along the distal tubule and collecting ducts, there is net secretion
of K which is stimulated by aldosterone and when there is dietary
K excess. Along the distal tubule and collecting ducts, there is net
secretion of K which is stimulated by aldosterone and when there
is dietary K excess
In the CD, K secretion is by the principal cells (via luminal K
channels and basolateral Na-K ATPase) and K reabsorption is by
the alpha intercalated cells via a luminal H-K ATPase
Renal regulation of Potassium
Giebisch, G. Am J Physiol Renal Physiol 274: F817-F833 1998
Copyright ©1998 American Physiological Society
Main features of K+ transport,
based on clearance experiments
1. K+ secreted by renal tubules (excreted K+> filtered K+)
2. K+ excretion can be dissociated from the rate of
glomerular filtration
3. Reabsorption of K+ along the nephron precedes K+
secretion
4. Secretion of K+ occurs by exchange for Na+-adequate
Na+ reabsorption is necessary for effective K+ secretion
5. Reciprocal relation between urinary excretion of K+ and
H+, carbonic anhydrase inhibitors induce kaliuresis
6. Adrenal steroids stimulate K+ secretion
FROM:
A trail of research on potassium
Gerhard H Giebisch. Kidney International (2002) 62, 1498–1512; doi:10.1046/j.1523-1755.2002.t01-2-00644.x
K secretion from principal cells
into the CD lumen
It is enhanced by :
Luminal determinants:
1- increases in tubule urine flow
2- the delivery of sodium to the CD
3- the delivery of poorly reabsorbed anions
(other than Cl) to the CD
Cellular determinants: the activity and
abundance of K channels at the luminal cell
membrane and of Na-K ATPase at the
basolateral membrane
K secretion from principal cells into the CD lumen
Giebisch, G. Am J Physiol Renal Physiol 274: F817-F833 1998
Copyright ©1998 American Physiological Society
Function of renal potassium
channels
1) Maintenance of negative potential of
tubule cells
2) Regulation of volume of tubule cells
3) Recycling across apical and basolateral
cell membranes to supply potassium to Na2Cl-K cotransport and Na-K-ATPase
4) Potassium secretion in initial and
cortical collecting tubule
Cell model of a principal cell with overview of
factors known to regulate K secretion
Factors involved in the regulation of K transport by aldosterone and peritubular K:
(1) Changes in peritubular K increase apical K and Na channel activity, stimulate
Na,K-ATPase activity, and augment the basolateral membrane area. High K also
activates the release of aldosterone.
(2) Changes in aldosterone stimulate apical Na channels but enhance K channel
activity only during chronic hyperkalemia. Similar to high K, aldosterone stimulates
Na,K-ATPase activity and increases the basolateral membrane area and Na,K-ATPase
activity.
Hyperkalemia and Hypokalemia
Serum potassium is normally
maintained between 3.5 -5.0 mmol/L
Hyperkalaemia is defined as a
potassium level greater than 5.5
mmol/L
Hypokalemia is defined as a
potassium level less than 3.5
What is your diagnosis?
Hyperkalemia
common laboratory abnormality complicating between
1.1% and 10.0% of all hospital admissions
occurs in as many as 11% of patients using
angiotensin-converting enzyme inhibitors (ACEIs)
Without warning, hyperkalemia may cause nearly any
dysrhythmia
Estimates of deaths caused by hyperkalemia in the
general population are unavailable
in patients with end-stage renal disease in the United
States, hyperkalemia accounted for 1.9% of mortality
in 1993
Arch Intern Med. 1998;158:917-924.
Causes of Hyperkalemia
Excessive exogenous potassium load (Increased Intake)
Potassium supplements (IV or Oral)
Excess in diet
Salt substitutes (e.g. potassium salts of penicillin)
Haemolysis
Rhabdomyolysis
Extensive burns
Tumor Lysis Syndrome
Intense physical activity
Trauma (especially crush injuries and ischaemia)
Acidosis (metabolic or respiratory)
Insulin deficiency
Drugs
Excessive endogenous potassium load (Increased Production)
Redistribution (Shift from intracellular to extracellular fluid)
Succinylcholine
Beta-blockers
Digoxin (acute intoxication or overdose)
Hyperkalemic familial periodic paralysis
Decreased glomerular filtration rate (eg, acute or end-stage chronic renal failure)
Decreased mineral corticoid activity
Defect in tubular secretion (eg, renal tubular acidosis IV)
Drugs (eg, NSAIDs, cyclosporine, potassium-sparing diuretics, ACE Inhibitors)
Diminished potassium excretion(Decreased Excretion)
Causes of pseudohyperkalaemia
(Factitious, spurious )
-Related to collection and storage of specimen:
Difficulty in collecting sample
Patient clenched fist when sample was taken
Sample was shaken or squirted through needle into
collection tube
Contamination with anticoagulant from another sample
(potassium EDTA)
Cooling
Deterioration of specimen due to length of storage
-Pre-existing conditions:
Thrombocytosis
Severe leucocytosis (which can also produce
pseudohypokalaemia)
Hereditary and acquired red cell disorders
True or pseudo hyperkalaemia?
Identify patients at risk of having true rather than spurious
hyperkalaemia or signs or symptoms of hyperkalaemia
Patients with known chronic kidney disease
Patients taking drugs that raise potassium (notably
angiotensin converting enzyme inhibitors, angiotensin receptor
blockers, potassium sparing diuretics, potassium salts),
trimethoprim, β blockers, and non-steroidal anti-inflammatory
agents.
Patients with obstructive uropathy
Patients with clinical features such as myopathy, paralysis,
arrhythmias, bradycardia
Patients at greater risk from severe hyperkalaemia: those
aged over 70 and those with elevated serum urea.
Patients with acute illness (acute renal failure, ketoacidosis,
etc)
Consider spurious hyperkalaemia in the absence of all the above
Clinical manifestations of
hyperkalemia
- Patients may have symptoms
related to the cause of the
hyperkalemia(eg. polyuria
and polydipsia with
uncontrolled diabetes)
- Serious manifestations usually
occur when the serum K+ is
≥7.0 meq/L (chronic
hyperkalemia) or possibly at
lower levels with an acute
rise in serum potassium
Cardiac manifestations
The progression and severity
of ECG changes do not
correlate well with the serum
potassium concentration
Illustration of a normal action potential (solid line)
and the action potential as seen in the setting of
hyperkalemia (interrupted line).
Severe muscle weakness or
paralysis
Ascending muscle weakness (can
progress to flaccid paralysis,
mimicking Guillain-Barré)
Sphincter tone and cranial nerve
function are typically intact
Respiratory muscle weakness is rare
Resolve with correction of the
hyperkalemia
Hyperkalemic periodic paralysis
Autosomal dominant mutations in the
skeletal muscle cell sodium channel
Mutations of the skeletal muscle sodium
channel gene SCN4A, which is located on
chromosome 17q23-25
prevalence of 1:200,000. Women and men
appear to be equally affected
transient episodes of paralysis
precipitated by cold exposure, rest after
exercise, fasting, or the ingestion of small
amounts of potassium
Treatment of Hyperkalemia
patients with mild elevations in
potassium concentration could be
treated as outpatients
those patients with objectively severe
or life-threatening hyperkalemia
would be hospitalized
Treatment options for
hyperkalemia
When arrhythmias are present, a wealth of anecdotal and
animal data suggests that IV calcium is effective in treating
arrhythmia
Inhaled beta-agonists, nebulised beta-agonists, and
intravenous (IV) insulin-and-glucose were all effective.
The combination of nebulised beta agonists with IV insulinand-glucose was more effective than either alone.
Dialysis is effective.
Results were equivocal for IV bicarbonate.
K-absorbing resin was not effective by four hours, and
longer follow up data on this intervention were not
available from RCTs.
2009 The Cochrane Collaboration. Published by John Wiley & Sons, Ltd.
Treatment options for
hyperkalemia
Treatment
Usual dose
Route of administration
Onset/duration
1-2/10-30 min
Expected result
Calcium gluconate 1 g (4.4 mEq)
IV over 5 min
Reversal of cardiac toxicity
Calcium chloride 1 g (13.5 mEq)
Central IV over 5-10 min 1-2/10-30 min (Note: no effect on K+ levels)
Insulin (regular) 1 unit/3-5 g dextrose
IV bolus or infusion
10-20 min/2-6 h
Shift of K+
Dextrose 50 mL D50W (25 g)
IV over 5 min
30 min/2-6 h
Shift of K+ intracellularly
0.5-1.0 L D10W
IV over 1-2 h
Maintains blood glucose
Avoid if hyperglycemic
Salbutamol/albuterol 0.5%
10-20 mg
Nebulized over 10 min (diluted)
30 min/1-2 h
Shift of K+
Not as monotherapy
Sodium bicarbonate 50-100 mEq
IV bolus or infusion
Effects unreliable
Sodium polystyrene sulfonate 15-60 g
30-60 min/2-6 h
Orally or rectally
Furosemide
20-80 mg
IV bolus or infusion
Hemodialysis
–
–
1-6 h/variable
5-30 min/2-6 h
Immediate/variable
Shift of K+ intracellularly
Nonrenal elimination of K+
Renal elimination of K+
Increased elimination of K+
Hypokalemia
Hypokalemia is found in over 20 percent of
hospitalized patients
Low serum potassium concentration has been found in
10 to 40 percent of patients treated with thiazide
diuretics
The first step in the management of hypokalemia is to
review the patient's drug record.
Etiologies:
Decreased intake (normal range of potassium intake
is 40 to 120 meq per day)
Increased translocation into the cells (usually by the
Na-K-ATPase pump in the cell membrane)
Most cases result from unreplenished gastrointestinal
or urinary losses
Topiramate
Anticonvulsant
Partial onset seizure (monotherapy) and
primary generalized tonic-clonic seizure
(monotherapy)
Migraine prophylaxis
Partial onset seizures (adjunctive therapy)
Primary generalized tonic-clonic seizures
(adjunctive therapy)
Cluster headache (unlabeled use)
Neuropathic pain (unlabeled use)
Role of CA isoforms in the kidney and structure of topiramate.
Sacré A et al. Nephrol. Dial. Transplant. 2006;21:2995-2996
© The Author [2006]. Published by Oxford University Press on behalf of ERA-EDTA. All rights
reserved. For Permissions, please email: journals.permissions@oxfordjournals.org
Topiramate
Serum bicarbonate decreased (dose related: 7% to
67%; marked reductions [to <17 mEq/L] 1% to 11%)
due to inhibition of carbonic anhydrase and increased
renal bicarbonate loss
metabolic acidosis (hyperchloremia, nonanion gap)
renal tubular acidosis risk: increased in patients with a
predisposing condition (renal, respiratory and/or
hepatic impairment), ketogenic diet, surgery, diarrhea
,or concurrent treatment with other drugs which may
cause acidosis
Symptoms: fatigue, hyperventilation, distal
parasthesias, and confusion
Topiramate
Potential complications of chronic acidosis:
-nephrolithiasis (2-4 times that of the
untreated population ) due to lower urinary
citrate excretion
-osteomalacia
-reduced growth rates in children
Dose reduction or discontinuation (by
tapering dose) in patients with persistent or
severe metabolic acidosis
If treatment is continued, alkali
supplementation should be considered
MANIFESTATIONS OF
HYPOKALEMIA
Severity is proportionate to the
degree and duration of the reduction
in serum potassium
Symptoms generally do not become
manifest until the serum potassium is
below 3.0 meq/L (unless the serum
potassium falls rapidly)
Symptoms usually resolve with
correction of the hypokalemia
MANIFESTATIONS OF
HYPOKALEMIA
Severe muscle weakness (begins in the lower extremities,
progresses to the trunk and upper extremities, and can
worsen to the point of paralysis )
Muscle cramps, rhabdomyolysis, and myoglobinuria
(Decreased potassium release due to profound hypokalemia
can diminish blood flow to muscles during exertion, leading
to ischemic rhabdomyolysis )
Respiratory muscle weakness (Respiratory failure)
Involvement of gastrointestinal muscles (ileus and its
associated symptoms of distension, anorexia, nausea, and
vomiting )
Cardiac arrhythmias and ECG abnormalities
Glucose intolerance (Hypokalemia reduces insulin secretion)
Renal abnormalities
Renal abnormalities
Impaired concentrating ability
Increased ammonia production
Increased bicarbonate reabsorption
Altered sodium reabsorption
Hypokalemic nephropathy
Elevation in blood pressure
EKG changes in hypokalemia
small or absent T waves
prominent U waves
first or second degree AV block
slight depression of the ST segment
sometimes slight to marked QT-prolongation:
torsades and VF can be induced.
presence of concomitant factors, such as
coronary ischemia, digitalis, increased beta
adrenergic activity, and magnesium depletion,
can promote arrhythmias
EKG changes in hypokalemia
DIAGNOSIS AND EVALUATION
History and physical
Identify underlying cause
Lab
EKG
At serum potassium concentrations
below 2.5 meq/L, severe muscle
weakness and/or marked
electrocardiographic changes may be
present and require immediate
treatment
Treatment of hypokalemia
Supplemental potassium administration is also the
most common cause of severe hyperkalemia in
patients who are hospitalized.
When potassium is given intravenously, the rate
should be no more than 20 mmol per hour, and the
patient's cardiac rhythm should be monitored.
Oral potassium is safer, because potassium enters the
circulation more slowly.
Give over a period of days to weeks to correct losses
fully.
Treatment of hypokalemia
potassium chloride:
should be used because of its unique effectiveness in the
most common causes of potassium depletion.
potassium phosphate:
used to replace phosphate losses
potassium bicarbonate:
only recommended when potassium depletion occurs in
the setting of metabolic acidosis
Treatment of hypokalemia
On average, serum potassium decreases by 0.3 mmol
per liter for each 100-mmol reduction in total-body
stores
No simple formula for calculating the amount needed
in patients in whom potassium loss is continuing
40 to 100 mmol of supplemental potassium chloride is
needed each day to maintain serum potassium
concentrations near or within the normal range in
patients receiving diuretics
use a second diuretic drug that inhibits potassium
excretion, such as amiloride, triamterene, or
spironolactone
ensure adequate dietary potassium intake
Renal regulation of Potassium
Giebisch, G. Am J Physiol Renal Physiol 274: F817-F833 1998
Copyright ©1998 American Physiological Society
Effect of extracellular fluid volume (ECFV) contraction on potassium
secretion
Giebisch, G. Am J Physiol Renal Physiol 274: F817-F833 1998
Copyright ©1998 American Physiological Society
TTKG IN HYPERKALEMIA
TTKG = [Urine K ÷ (Urine osmolality / Plasma osmolality)]
÷ Plasma K
two assumptions:
That the urine osmolality at the end of the cortical collecting
tubule is similar to that of the plasma, since equilibration
with the isosmotic interstitium will occur in the presence of
antidiuretic hormone
That little or no potassium secretion or reabsorption takes
place in the medullary collecting tubule.
The TTKG in normal subjects on a regular diet is 8 to 9, and
rises to above 11 with a potassium load
A value below 7 and particularly below 5 in a hyperkalemic
patient is highly suggestive of hypoaldosteronism