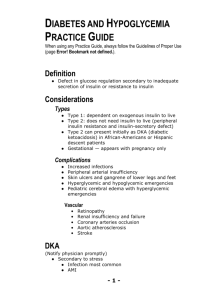
DKA
advertisement

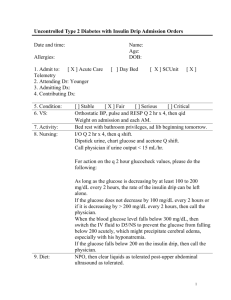
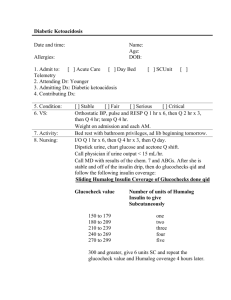
Diabetic Ketoacidosis Chief Complaint abdominal pain and vomiting History of Present Illness This 35 yo male presented with One day history of severe abdominal pain in epigastrium Sharp, constant ,radiating to the back accompanied by nausea Few episodes of non bloody vomiting without relief Patient denies same previous episodes, diarrhea, constipation, fever, sick contact, nobody at home had a same symptoms, no recent traveling Denies melena, blood in the stool Previous medical history DM type 2 HTN CAD S/P stent placement Familial Hypercholesterolemia Hypothyroidism and ETOH abuse Surgical hx none Allergy: NKDA Home Medications Metformine Lisinopril Clonidine Glyburide Levothyroxin Lopressor Nexium Plavix ASA Social History Lives at home with his mother Employe at Burger King Current smoker 4 cigarettes daily for 18 years Vodka 1 pint daily Denies illicit drug using Physical exam 35 year-old Hispanic Male appears alert, oriented and cooperative Vital Signs: Blood Pressure 131/96 Pulse 120 Respirations 20 No check for orthostatic BP/P Temperature 100.1 degrees Skin: Normal in appearance and texture Physical exam (cont'd) HEENT: Scalp normal Pupils equally round, 4 mm reactive to light and accommodation Sclera and conjunctiva normal External auditory canals normal. Nasal mucosa normal. Oral pharynx is normal without erythema or exudate. Tongue and gums are normal Physical exam (cont'd) Neck: Easily moveable without resistance No abnormal adenopathy in the cervical or supraclavicular areas Trachea is midline and thyroid gland is normal without masses Carotid artery upstroke is normal bilaterally without bruits No JVD Physical exam (cont'd) Chest: Lungs are clear to auscultation and percussion bilaterally no crackles , wheezing. CVS S1/S2 normal, no S# Abdomen: The abdominal exam revealed mild epigastric tenderness to palpation but no rebound tenderness or guarding Mild distention, bowel sounds are normal in quality and intensity in all areas No bruit No masses or splenomegaly are noted Physical exam (cont'd) Extremities: No cyanosis, clubbing, or edema are noted Peripheral pulses are normal Nodes: No palpable nodes in the cervical, supraclavicular, axillary or inguinal areas Genital/Rectal: Normal rectal sphincter tone No rectal masses or tenderness Stool is brown and guaiac negative. Pelvic examination reveals normal external genitalia Physical exam (cont'd) Neurological: Cranial nerves II-XII are normal Motor and sensory examination of the upper and lower extremities is normal. Gait and cerebellar function are also normal Reflexes are normal and symmetrical bilaterally in both extremities. Initial Problem List Abdominal pain Vomiting Fever, Tachycardia DM HTN ETOH abuse CAD Hyprecholesterolemia Laboratory results CBC WBC 14.8 HGB 13.1 HCT 38.3 Platelets 200 NEUT 84.0 UA CMP GLUCOSE 436 BUN 10.0 CR 1.3 NA 136 uprotein > 300 ur glucose >1000 Ketones >80 PH 7.18/22.6/24.6/8.3 K 6.8 CL 99 CO2 less 5 BIL 0.7 ALT 54 AST 27 Alk. Phosp. 217 Amylase 161 DKA Definition DKA is defined as a plasma glucose level >250 mg/dl, plasma bicarbonate <15 mEq/l, pH <7.35, ketonemia, and an elevation in the anion gap. This patient clearly meets the criteria for DKA based on his blood glucose of 436 mg/dl, CO2 of <5, pH of 7.18, anion gap of 32, and obvious ketonemia. Management: Phase 1 - Fluids 1. 2. Correct Volume Deficit 1. Protocol 1 (standard protocol) 1. Replace first 50% volume deficit in first 8 hours 1. Use Normal Saline or Lactated Ringers 2. Replace remaining 50% deficit over next 16 hours 1. Use D5 1/2 NS at 150-250 ml per hour 2. Protocol 2 1. NS at 10 cc/kg/hr (+/- 5 cc/kg/hr) 1. Until Serum Glucose <250 mg/dl 2. Then D5 1/2NS with 20 kcl 1. Give 150-250 cc/hour Precautions 1. Do not drop Serum Osmolality (calc) >3 mOsms/hour 1. Risk of cerebral edema 2. Slow replacement if Fluid Overload risk 1. Congestive Heart Failure 2. Chronic Renal Insufficiency 3. Myocardial Infarction 3. Follow Intake and output closely Management: Phase 2 - Acidosis, electrolytes 1. Potassium Replacement 1. Precautions 1. Hypokalemia must be corrected prior to Insulin 2. Hold Insulin until potassium >3.3 meq/L in adults 2. Prerequisites 1. Electrocardiogram without signs of Hyperkalemia 2. Adequate urine output 3. Administration: Adults 1. Serum Potassium <3.3 meq/L 1. Do not administer Insulin until potassium >3.3 2. Give KCl 40 meq/hour IV until corrects 1. Requires hourly recheck of Serum Potassium 2. This is maximum IV potassium rate! 3. Requires cardiac monitoring 2. Serum Potassium 3.3 to 5.0 meq/L 1. Standard replacement: 20-30 meq per liter 3. Serum Potassium >5.0 meq/L 1. Do not administer any potassium 2. Monitor every 2 hours until <5.0 Management: Phase 2 - Acidosis, electrolytes (cont'd) 2. Phosphate Replacement 1. Indications 1. Serum Phosphorus < 0.5-1.0 mg/dl (Severe Depletion) 2. Controversial - May not be required 3. Consider if cardiopulmonary adverse affects 2. Contraindications 1. Renal Insufficiency 3. Administration 1. Determine Potassium Replacement as above 2. Replace part of potassium with potassium phosphate 1. Potassium Phosphate: Replace one third potassium 2. Potassium Chloride: Replace two thirds potassium Management: Phase 2 - Acidosis, electrolytes (cont'd) 3. Magnesium Replacement 1. Indications 1. Symptomatic Hypomagnesemia (Magnesium <1 meq/L) 2. Administration 1. MgSO4 50%: 2.5-5.0 ml (20-40 meq) IM 4. Sodium Bicarbonate Replacement 1. Indications 1. ABG pH < 6.9 to 7.0 after initial hour of hydration 2. Other contributing factors 1. Shock or Coma 2. Severe Hyperkalemia Management: Phase 3 - Blood Glucose Control 1. Precautions 1. 2. Hypokalemia must be corrected prior to Insulin Adult Insulin protocol 1. IV Insulin administration 1. Initial 1. Give IV bolus of 0.15 units/kg 2. Start 0.1 units/kg/hour Insulin Drip 2. Maintenance 1. Anticipate Serum Glucose drop of 50-70 mg/dl/hour 1. If inadequate drop, then increase drip 2. Increase Insulin Infusion rate by 50-100% 3. Continue at increased rate until adequate 2. When Serum Glucose <200-250 mg/dl 1. Keep Serum Glucose at 150 to 200 mg/dl 2. Decrease rate by 50% (to 0.05 units/kg) or 3. Discontinue Insulin Drip and start SC dosing 2. IM or SC Insulin administration Management: Phase 3 - Blood Glucose Control (cont'd) 3. 4. Glucose monitoring 1. Glucose monitoring every 30 minutes to 1 hour 2. Target glucose decrease 50-70 mg/dl/h Dextrose Administration 1. Add 5% Dextrose to fluids when glucose < 250 mg/dl