Potassium disorders
advertisement

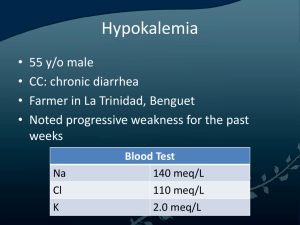
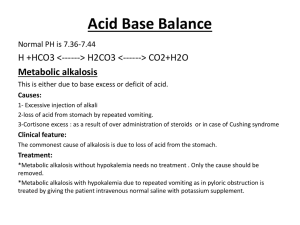
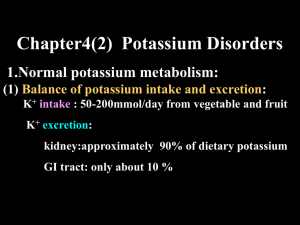
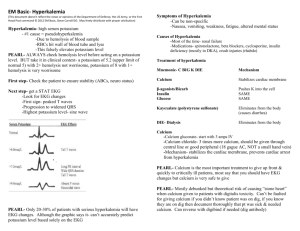
Potassium Disorders Dr Hala Ezzat Eid Professor of Anesthesia and Intensive care Ain Shams University Objectives: By the end of this lecture and reviewing ERC guidelines you should be able to: 1. Define normal serum K, hyper/hypokalemia. 2. Enumerate causes of hyper/hypokalemia. 3. Recognize hyper/hypokalemia 4. Discuss management of hyper/hypokalemia and if any modifications to BLS/AlS . Normal serum potassium Extracellular potassium concentration 3.5 and 5.0 mmoll−1 (mmol/L). N.B. 1mmol = 1mEq for univalent ions e.g. Na+, K+, HCO3 1mmol = 2 mEq for divalent ions e.g. Ca++, Mg++ So always use mmols Understanding Role of K in membrane potential Understanding Role of K in membrane potential Sodium is predominantly an extracellular cation while potassium is predominantly an intracellular cation Cell membrane is permeable to K but much less to Na, hence K+ diffuses down its concentration gradient out of the cell leaving behind negatively charged proteins. This leads to a potential difference across the membrane (a negative voltage on the inside relative to outside). . Understanding Role of K in membrane potential If K+ continued to leak out of the cell, its chemical gradient would be lost over time; however, a Na+/K+-ATPase pump brings the K+ back into the cell and thereby maintains the K+ chemical gradient (the pump moves three sodium ions out of the cell for every two potassium ions it puts in). Understanding Role of K in membrane potential During action potential Na+ channels open > Na+ enters the cells with reversal of membrane potential (positive IC) Repolarization takes place mainly by potassium leaving the cells. Thus K+ has an important role in repolarization. Where does potassium in blood come from? GIT intake Shift from ICF. (1) Insulin enhances potassium entry into cells (2) Beta-adrenergic agonists enhance potassium entry into cells. (3) Alkalosis enhances potassium entry into cells How does the body get rid of potassium? 1. Mainly RENAL excretion. Aldosterone stimulates potassium secretion and sodium and water retention . 2. GIT losses. 3. Shift into ICF N.B. In acidosis H+ increase in ECF, so H+ move into the cell and K+ move out of the cell in order to decrease the acidity. Beta-adrenergic agonists enhance potassium entry into cells (stimulates Na+-K= ATPase) Understanding diabetic ketoacidosis: Total body water (TBW) constitutes 60% of total body weight. For a 70 kg man, TBW = 0.6 x 70 = 42 L Understanding body fluid compartment Total body water (TBW) constitutes 60% of total body weight. For a 70 kg man, TBW = 0.6 x 70 = 42 L Understanding ACEIs Hyperkalaemia This is the most common electrolyte disorder associated with cardiopulmonary arrest. Serum K concentration higher than 5.5mmoll−1 Severe hyperkalaemia serum K > 6.5mmoll−1. Causes of hyperkalemia: GIT Diet IC compartment Tissue breakdown (rhabdomyolysis, tumour lysis, haemolysis), Stored Packed red blood cells Renal Renal failure Aldosteron Addisons ACE-I NSAIDs K sparing diuretics Metabolic acidosis, beta-blockers, Insulin deficiency N.B. Hemolysis of blood sample can cause Pseudohyperkalemia, because of the use of torniquet >> recheck in stable patients without a risk of hyperkalemia. Hyperkalemia Excitable Tissues Effect Nerve paraesthesia, depressed deep tendon reflexes Sk Muscles Weakness, paralysis, respiratory failure Cardiac ms ECG abnormalities, arrhythmias, cardiopulmonary arrest or sudden death Hyperkalemia Tall, peaked T waves Flattened P waves Prolonged Widened PR interval QRS Arrhythmias, cardiac arrest N.B. T wave represents ventricular repolarization High serum K >> High T wave Treatment of hyperkalaemia There are three key treatments for hyperkalaemia5: 1. cardiac protection; 2. shifting potassium into cells; 3. removing potassium from the body. Treatment of hyperkalaemia CALL FOR HELP Treatment of hyperkalaemia Cardiac protection (In presence of ECG changes) Calcium chloride (10%): 10 ml IV over 2 to 5 minutes. It reduces the effects of potassium at the myocardial cell membrane and lowers risk of VF. Treatment of hyperkalaemia Shifting potassium into cells: 1. Glucose / insulin: 25 g glucose (50 mL of D50 or 100 ml D25) and 10 U regular insulin given IV over 15 to 30 minutes (onset 15–30 min) 2. Salbutamol 5mg nebulised. Several doses (10–20 mg) may be required (onset 15–30 min) 3. Sodium bicarbonate: 50 mmol IV over 5 minutes if metabolic acidosis present (onset 15–30 min). Treatment of hyperkalaemia Promote potassium excretion: 1. Diuresis: furosemide 40 to 80 mg IV 2. Potassium exchange resins 3. Dialysis Hypokalaemia Serum Severe potassium < 3.5mmoll−1. hypokalaemia is defined as a K+ < 2.5mmoll−1 Causes of hypokalemia IC compartment Renal Aldosteron GIT -Poor dietary intake -GIT loss (diarrhoea) laxatives -Metabolic alkalosis Renal losses (DI) -Beta-agonists Dialysis -Insulin therapy Diuretics -Cushing’s Syndrome -Hyperaldosteronism -Steroids C/P hypokalemia Excitable Tissues Effect Sk Muscles weakness, cramps rhabdomyolysis, respiratory failure. Smooth ms constipation. Cardiac ms ECG abnormalities, arrhythmias, cardiopulmonary arrest or sudden death Hypokalemia U waves T wave flattening ST-segment changes Arrhythmias, cardiac arrest Hypokalemia N.B. The maximum recommended IV dose of potassium is 20 mmol per hour in an adult with continuous ECG monitoring during infusion. Better via a central line. If using a peripheral line dilute in 500 ml ringer. Reassess by measuring serum K. In severe hypokalemia >> give magnesium 4 mmol (2 gm ) over 15 minutes i.v.i. Hypokalemia N.B> Rapid infusion (10 mmol over 5 minutes and repeat once if needed, followed by 10mmol 10min if needed) is indicated for unstable arrhythmias when cardiac arrest is imminent.