Palliative Care in the Acute Setting

Oral Care
Aims
By the end of the session the participant will:
Be familiar with the structures within and around the mouth
Be aware of the negative impact on general health which can occur due to poor oral health
Know the correct equipment to use when carrying out oral care
Oral Care
Poor oral hygiene is a common cause of distress for patients and families
Poor care may be due to lack of training, knowledge, inconsistent care
Not always a high priority
Essential for patient comfort
Risk Factors
for
Oral
Complications
Systemically ill, terminal illness, unconscious patient, tracheostomy
Oxygen therapy, mouth breathing, nil by mouth.
Naso – gastric/peg feeding
Chemotherapy/radiotherapy, drug therapy
Ill fitting dentures
Diabetes
Dementia
Consequences of poor oral care
Pneumonia
Septicaemia
Endocarditis
Pain
Xerostomia (dry mouth)
Halitosis
Difficulty eating and drinking
Withdrawal
Low mood
Good Oral Care
Frequent inspection important using a pen torch, tongue depressor and gloved finger
Have an understanding of the possible risk factors
Examine in and outside the mouth
Early detection/reporting of problems
Need instruction on specific requirements for that patient
Dentate Patients (own teeth)
Brush teeth at least twice per day with toothbrush and fluoride toothpaste
Moisturise lips if necessary with a water based lubricating gel
ONLY use foam swabs soaked in water if using a toothbrush is too painful or impossible,
Care of Dentures
Remove and brush with a toothbrush and water after every meal
Rinse mouth with water to remove debris
Moisturise lips if necessary with water based lubricating gel
Remove and soak overnight in water
If oral infection is present, e.g. candida, dentures should be soaked in 1% sodium hypochlorite solution 2ml mixed with 160ml of tap water. If they have metal parts – soak in chlorhexidine 0.2%
Oral Problems
Candida (thrush)
Bacterial infections
Xerostomia (dry mouth)
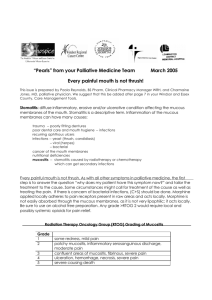
Mucositis
Cold sores
Ulcers
Angular cheilitis
Candida
Dry mouth
What causes a dry mouth?
What problems can a dry mouth cause?
Causes
Drugs – lots of them
Radiotherapy
Oxygen
Mouth breathing
Complications of dry mouth
Decay
Gum recession and loss of teeth
Difficulty eating
Difficulty speaking
Trauma of mucosa
Halitosis
Dry Mouth
(
Xerostomia
)
Continue brushing teeth twice per day with fluoride toothpaste
Sips of and rinsing with tap water
Artificial saliva – Avoid glandosane in patients with their own teeth
Saliva Orthana has a porcine extract so is not suitable for some patients due to culture
Oral balance gel
Sugar free chewing gum
Review of medication
Cold sore
Aphthous ulcer
Angular cheilitis
Treatment of Painful Mouths
Some patients may need pain relief such as cocodamol or even morphine in severe cases
Avoid strong, acidic mouthwashes e.g. brand makes
Benzydamine (Difflam) mouth wash has local anaesthetic. It can be diluted 1:1 if stinging
Topical steroid for ulcers such as hydrocortisone pellets