bacterial keratitis - Pennsylvania Optometric Association

ALAN G. KABAT, OD, FAAO
MEMPHIS, TN alan.kabat@alankabat.com
JOSEPH SOWKA, OD, FAAO
FT. LAUDERDALE, FL
ANDREW GURWOOD, OD, FAAO
PHILADELPHIA, PA jsowka@nova.edu
agurwood@salus.edu
Course Description: Case presentations provide a springboard for in-depth discussion of several challenging anterior segment conditions. Emphasis is placed on understanding the presentation, pathophysiology and management of the various clinical entities.
Learning Objectives/Outcomes: At the conclusion of this course, the attendee will be able to:
1.
Identify the pathophysiology, clinical presentation and management of bacterial keratitis;
2.
Identify the pathophysiology, clinical presentation and management of dacryoadenitis;
3.
Identify the pathophysiology, clinical presentation and management of corneal laceration;
4.
Identify the pathophysiology, clinical presentation and management of uveitis, as well as the essential laboratory work up;
5.
Identify the pathophysiology, clinical presentation and management of herpes simplex keratitis;
6.
Identify the pathophysiology, clinical presentation and management of recurrent corneal erosion.
BACTERIAL KERATITIS
Breakdown of corneal defenses (dry eyes, corneal trauma, corneal hypoxia, etc.)
Introduction of pathogen (corneal abrasion mismanagement, contact lenses, etc.)
Proliferation of organisms and release of toxins and proteolytic enzymes
Antigen-antibody reaction
Stromal edema (splitting of stromal collagen lamellae sheets)
Cellular transudation and emigration
Infiltration
Phagocytosis of organisms with proteolytic enzyme release and stromal lysis
Antigenic neutralization (hopefully)
Cicatrization (fibroblastic proliferation of scar tissue)
Visual loss
Clinical Picture of Bacterial Keratitis
Pain, photophobia, lacrimation
Profound conjunctival and episcleral injection
Involvement of innocent bystanding tissue
Anterior chamber reaction
Possible (sterile) hypopyon
Focal infiltrate with overlying epithelial staining and breakdown
The spectrum of clinical findings is broad (from an initially mild, often misdiagnosed presentation of S. aureus to the exaggerated presentation of Pseudomonas)
Any staining infiltrate should be presumed to be an infectious ulcer until proven otherwise
Management of Bacterial Keratitis
Cultures and sensitivity studies
Broad spectrum antibiosis: Fluoroquinolones
1.
Ciprofloxacin (Ciloxan) ii gtt Q15min X 6hrs, then ii gtt Q 30min X 18 hrs.
2.
Ocuflox Q30 minutes while awake, and then BID at night is as effective as fortified antibiotics.
3.
Levofloxacin (Quixin)?
4.
New alternatives- fourth generation fluoroquinolones: Vigamox/ Moxeza
(moxafloxacin); Zymar/ Zymaxid (gatifloxacin) – Q1H
Equal gram (-) coverage, greater gram (+) coverage than earlier generation fluoroquinolones
5.
Newest options: Besivance (besifloxacin) , Moxeza (moxifloxacin) , Zymaxid (gatifloxacin)
Cycloplegics (scopolamine 0.25% TID or atropine 1% BID) - decreases blood-aqueous barrier breakdown
Corticosteroids (reduces inflammation by constricting blood vessel walls and reducing vessel wall permeability. Also blocks prostaglandin formation and release and stabilizes lysosomal membranes).
Use corticosteroids only if step 1 is successfully completed (clinical impressions vs. microbiologic study results).
DACRYOADENITIS
Inflammation of the lacrimal gland
Usually seen in younger adults
May be acute or chronic: o Acute form presents with greater pain, redness & symptomology; usually infectious in nature (bacterial or viral) o Chronic form is more common; usually inflammatory & due to underlying systemic autoimmune disease (e.g. sarcoidosis, Sjögren's syndrome, systemic lupus erythematosus, Wegener's granulomatosus)
Acute Dacryoadenitis - o Typically unilateral o Ocular redness, tearing, & swelling of the upper lid o Painful proptosis & ophthalmoparesis o May have associated preauricular lymphadenopathy & fever
Chronic Dacryoadenitis - o Usually bilateral o S-shaped swelling to outer ⅓ of the eyelid o Pain is variable o Swollen lacrimal gland is often evident on lid retraction
Dacryoadenitis: Diagnostic management o Orbital CT or MRI o Laboratory studies o CBC with differential o Serology based on history & associated symptoms (e.g. ACE, FTA-ABS, RPR, PPD with anergy panel) o Transcutaneous, transeptal biopsy should be performed in recalcitrant cases of dacryoadenitis or when a malignant process is suspected
Dacryoadenitis: Therapeutic Management o Acute - warrants systemic antibiotics
Amoxicillin (250-500 mg po q8h)
Cephalexin (250-500 mg po q6h)
In more severe cases, hospitalization with IV antibiotics may be necessary o Chronic dacryoadenitis may be managed with a course of systemic steroids
Typical therapy involves 80-100 mg of oral prednisone daily for 1-2 weeks, followed by slow taper.
PENETRATING INJURY: CORNEAL LACERATION
Excessive PAIN, decreased vision
Deeper than abrasion; may be smaller, linear
+ Seidel’s sign; additionally, may see hyphema, A/C rxn, flattened A/C (relative), air bubbles in A/C
Iris prolapse possible
IOP is low -- DO NOT perform tonometry!
Management o Photodocument (if possible for clinicolegal purposes) o MINIMAL manipulation of the globe! o Avoid topical medications! o Shield the eye but DO NOT PATCH! o N.P.O. o Refer IMMEDIATELY for surgical repair
ANTERIOR UVEITIS
Associated factors o An inflammation of the iris and ciliary body o May result from direct trauma to the eye (most often) o May occur as a result of inflammation of other ocular structures (e.g., keratitis, scleritis) o May be associated with underlying systemic disease (including but not limited to):
ankylosing spondylitis
Behçet’s disease
inflammatory bowel disease
juvenile rheumatoid arthritis
Reiter’s syndrome
sarcoidosis
syphilis
tuberculosis
Lyme disease o Improper management may result in secondary, inflammatory glaucoma o
Signs and Symptoms o Signs:
Variable redness
Ptosis or blepharospasm (due to discomfort)
Tearing
Visual acuity normal to mildly reduced
20/40 or better in most cases
More difficulty with near / accommodative tasks
o Symptoms:
Deep, dull “achy” pain in affected eye and orbit
Extreme photophobia
“Hazy” vision
Biomicroscopic evaluation o Mild lid congestion (pseudoptosis); palpebral conjunctiva is unaffected o Circumlimbal “flush” , i.e., injection of the episclera and conjunctiva concentrated around the cornea o Mild corneal edema o Keratic precipitates in chronic conditions (“granulomatous”) o Anterior chamber “cells & flare” **
“cells” = white blood cells liberated from uveal blood vessels
“flare” = proteinaceous by-products of inflammation o Posterior or (less commonly) anterior synechia o Iris nodules o Altered intraocular pressure
Initially reduced because of secretory hypotony
Inflammatory by-products clog the trabecular meshwork, inducing IOP elevation
May range from 30 to 80 mmHg in extreme cases
Management o 2 primary goals:
1.
immobilize the iris & ciliary body to decrease pain and prevent exacerbation
2.
quell the inflammatory response to prevent ocular sequelae o STRONG topical cycloplegics
Choice of drug dependent upon severity of reaction, iris color, and presumed patient compliance
Best choices include
¼% scopolamine
1% atropine o Topical corticosteroids
Must be deeply penetrating and efficacious
Must be given FREQUENTLY, particularly during early stages of treatment
Drug choices include:
difluprednate **
prednisolone acetate
loteprednol ? o Address synechiae using 1% atropine + 10% phenylephrine topically o Elevated IOP should be addressed using standard topical antiglaucoma therapy:
-blockers (e.g., Timoptic
, Betoptic
)
CAIs (e.g., Trusopt
)
Prostaglandin analogs (e.g., Xalatan
) offer no clinical benefit
Miotics (e.g., pilocarpine) are ABSOLUTELY CONTRAINDICATED
o In recurrent cases (i.e., two or more similar presentations), a thorough medical evaluation to ascertain underlying etiology is indicated
CXR
Sacroiliac joint films
Serology:
CBC with differential
ESR
ANA
HLA-B27
RF
ACE
FTA-ABS
Lyme titer
HERPES SIMPLEX KERATITIS
Pathophysiology:
Initial infection by herpes simplex virus occurs in childhood (hand to eye, mouth to eye)
After initial infection, virus enters a dormant phase in cell ganglia
"Trigger factors" induce reactivation of viral replication throughout the patient's life; include: fever, emotional stress, exposure to UV radiation, menstruation, trauma, immunosuppression
About half of all infected patients experience re-activation within 5 years
Most commonly ocular manifestion is dendritic epithelial keratitis
More severe presentations can manifest as geographic epithelial keratitis
Clinical presentation - dendritic keratitis:
Branching epithelial ulcer; may begin as nondescript punctate epitheliopathy
Stains centrally with NaFl, peripherally with rose bengal or lissamine green ("terminal end-bulbs")
Associated conjunctival injection, edema; uveitis possible
Recurrent attacks lead to corneal hypoesthesia, i.e. diminished corneal sensitivity
(+) Cotton-wisp test
Patients may be far less symptomatic than predicted by ocular appearance
Management:
Herpes virus cannot be eradicated; management efforts are aimed at suppression and amelioration of symptoms
Historical tandard of care in U.S. is topical trifluridine 1% q2h - 9 times daily, tapered to q3-4h as ulcer shows signs of closure; maintain at QID for at least 7-10 days.
More recent option is ganciclovir 0.15% ophthalmic gel 5 times daily until resolution, then reduced to TID for 7 days
Oral acyclovir may be used in patients who lack dexterity or compliance with topicals
(400 mg po five times daily)
Corticosteroids are absolutely contraindicated in active epithelial infection
Herpetic Eye Disease Study (HEDS) 1998: Acyclovir 400 mg po BID X 12 months may reduce rate of recurrence by as much as 50%
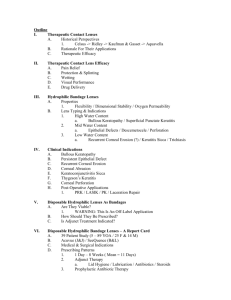
RECURRENT CORNEAL EROSION
History, History, History
History of Corneal Abrasion
Previous episodes of RCE
Pain on awakening
A breakdown of the epithelial layer of the cornea due to a breach in the integrity of the basement membrane
Common Etiologies:
Corneal dystrophy (e.g. granular dystrophy)
Trauma; often follows improperly treated corneal abrasion
Can present as a small epithelial defect or as a large abrasion
Treatment
Bandage SCL
Pressure patching in rare instances
Prophylactic ntibiotic
Cycloplegic
Artificial Tears and Hypertonic agents
Anterior Stromal Puncture (ASP)
Oral doxycycline + topical steroids
Amniotic membrane… ?