Physician Assistant Protocols
advertisement

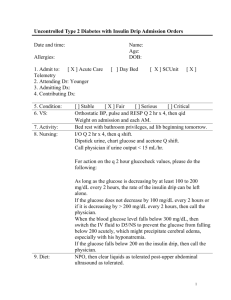
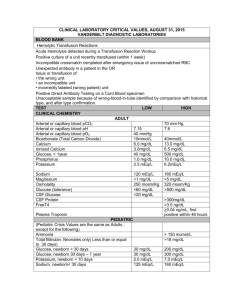
DIABETES AND HYPOGLYCEMIA PRACTICE GUIDE When using any Practice Guide, always follow the Guidelines of Proper Use (page Error! Bookmark not defined.). Definition ● Defect in glucose regulation secondary to inadequate secretion of insulin or resistance to insulin Considerations Types ● Type 1: dependent on exogenous insulin to live ● Type 2: does not need insulin to live (peripheral insulin resistance and insulin-secretory defect) ● Type 2 can present initially as DKA (diabetic ketoacidosis) in African-Americans or Hispanic descent patients ● Gestational — appears with pregnancy only Complications ● ● ● ● ● Increased infections Peripheral arterial insufficiency Skin ulcers and gangrene of lower legs and feet Hyperglycemic and hypoglycemic emergencies Pediatric cerebral edema with hyperglycemic emergencies Vascular • • • • • Retinopathy Renal insufficiency and failure Coronary arteries occlusion Aortic atherosclerosis Stroke DKA (Notify physician promptly) ● Secondary to stress ● Infection most common ● AMI -1- ● ● ● ● ● ● ● ● ● ● Pregnancy ● Surgery Average adult fluid deficit is 6–10 liters (osmotic diuresis) Plasma glucose > 250 mg/dL (usually > 350 mg/dL) Adjustment to serum Na (sodium) levels — each additional 100 mg% over plasma glucose of 100 add 1.6 mEq/L to serum Na levels Potassium body deficit can be severe despite initial normal serum level (a decrease of 0.3–0.7 mEq/L for each decrease of pH of 0.1) ● Total body potassium deficit is 3–5 mEq/kg IV PO4 (phosphorous) may be needed if respiratory failure occurs Arterial pH < 7.3 (with venous pH add 0.03 if used instead of ABG) Serum osmolarity > 320 mOsm/L Serum bicarbonate < 18 Moderate ketonuria or ketonemia Symptoms and findings (some or all) ● ● ● ● ● ● ● ● ● Weakness Weight loss Mental status changes Dry mucous membranes Tachycardia Nausea and vomiting Abdominal pain Kussmaul respirations (deep rapid breathing) Peripheral vasodilatation can cause normothermia or hypothermia despite infection Evaluation ● ● ● ● ● ● CBC BMP Accucheck Chest x-ray U/A ABG or venous pH (add 0.03 to adjust to arterial pH) ● Blood, urine or infected site cultures if infection suspected Serum osmolality • If < 320mOsm/L, look for another cause of altered mental status • Osmolol gap > 10–20; suspect substance ingestion (normal < 10) Gap = Osmolality measured – Osmolality calculated (Osmolality calculation equation: 2(Na+K) + glucose/18 + BUN/2.8; normal 280–300mOsm/L) Ethanol mg%/4.6 is added to osmolol gap equation if present Gap > 50 carries high specificity for toxic alcohol such as methanol, ethylene glycol, or isopropyl alcohol Normal gap < 10 Fluid therapy Adult • IV NS infused 15–20 cc/kg/hour (1–1.5 liters average) • Continue NS if corrected Na is low • 0.45% NS at 4–14 cc/kg/hour after bolus infusion if “corrected” Na is normal or high • Add potassium 20–30 mEq/L when serum K reaches < 5.3 mEq/L (if urine output 0.5–1 cc/kg/hour) Pediatric (< 16 years of age) • IV NS 10–20 cc/kg/hour; may repeat prn; should not exceed 50 cc/kg total over 4 hours • Continued IV with 0.45% or NS at 5 cc/kg/hour after initial fluid therapy • If altered mental status acutely occurs, suspect cerebral edema (treatment 1–2 gms/kg mannitol IV — per physician) Insulin therapy ● Start after IV fluids given for one hour ● Check K+ level first (can cause K+ to drop; can be dangerous if already low; should be at least 3.3 mEq/L) Adults • Bolus 0.15 units/kg IV and/or continuous infusion 0.1 unit/kg/hour (up to 5–7 units/hour) • Should decrease plasma glucose 50–75 mg%/hour (if not, check hydration status) Pediatrics • Insulin bolus not recommended • Continuous infusion same as adult Potassium ● Add potassium 20–40 mEq to each liter of IV fluids when serum K+ < 5.3 mEq/L if urine output 0.5–1 cc/kg/hour or initial potassium < 3.3 mEq/L • Serum K+ 4.5−5.2 mEq/L give 10 mEq/hour IV • Serum K+ 3.0−4.5 mEq/L give 20 mEq/hour IV • Serum K+ initially < 3.0 mEq/L hold off starting insulin and give potassium IV per physician Consult criteria ● All DKA patients after initial assessment Hyperglycemic Hyperosmolar Syndrome (HHS) ● ● ● ● ● ● ● ● ● Develops over days or weeks Plasma glucose > 600 Serum osmolality > 320 mOsm Profound dehydration: adult 8–12 liters fluid deficit Small amount of ketonuria; small or absent ketonemia Serum bicarbonate > 15 Arterial pH > 7.3 Some alteration of consciousness Higher mortality than DKA Associated medications contributing to HHS ● ● ● ● ● ● Diuretics Propranolol Calcium channel blockers Dilantin Cimetadine Corticosteroids Evaluation ● Same as for DKA Treatment options ● IV NS 10–20 cc/kg/hour; may repeat prn; should not exceed 50 cc/kg total over 4 hours ● Continued IV with 0.45% or NS at 5 cc/kg/hour after initial fluid therapy ● Add D51/2NS or D5NS when plasma glucose reaches 300 mg/dL ● Start insulin infusion 0.1 unit/kg/hour (up to 5–7 units/hour) after first hour of IV fluid therapy • Insulin doses often lower than used in DKA Potassium treatment • Add potassium 20–40 mEq to each liter of IV fluids when serum K+ < 5.3 mEq/L if urine output 0.5–1 cc/kg/hour or initial potassium < 3.3 mEq/L Serum K+ 4.5−5.2 mEq/L give 10 mEq/hour IV Serum K+ 3.0−4.5 mEq/L give 20 mEq/hour IV Serum K+ initially < 3.0 mEq/L hold off starting insulin and give potassium IV per physician Consult criteria ● All cases Hypoglycemia Differential diagnosis ● ● ● ● ● CVA TIA Epilepsy Multiple sclerosis Psychosis Considerations Caused by: • Accidental or intentional overdose of diabetic medications • Sepsis • Alcohol use • Decreased caloric intake Symptoms • Severity symptoms depends on glucose level and rate of glucose decline • Symptoms may be masked by betablockers • Altered and decrease mental status • Sweating • Shaking • Anxiety Evaluation ● History and physical exam ● Medication and food intake history ● Accucheck every 30 minutes 2 hours or longer until stable glucose levels achieved ● BMP ● CBC if infection suspected ● Chest x-ray if pneumonia or aspiration suspected, or hypoxic ● U/A if infection suspected Treatment options ● Awake and alert: complex calorie intake PO ● Altered mental status: IV D50W 1 amp adults (100 calories) ● D25W ― 1 gm/kg in pediatrics not to exceed adult dose ● D12.5W for neonates (1 gm/kg) ● D10W drip at 75–100 cc/hour (adult) if repeat D50W boluses needed for recurrent hypoglycemia or hypoglycemic agent overdose ● Glucagon 1 mg IM if no IV access • May not work with depleted glycogen stores in malnutrition Liver disease Alcoholics Neonates ● Octreotide can be used in sulfonylurea refractory hypoglycemia (consult physician) ● Hydrocortisone IV for adrenal insufficiency Discharge criteria ● Stable glucose levels in diabetic patients on preexisting insulin therapy ● Good home support ● Reliable patient Discharge instructions • Hypoglycemia aftercare instructions • Follow up with primary care provider within 12–24 hours Consult criteria ● Oral hypoglycemia therapy (usually need admission) ● Fasting hypoglycemia on no diabetic medication ● Intentional insulin overdose ● Poor home situation ● Abnormal vital signs ● Continued altered mental status ● Significant comorbidities (cancer, hepatic disease, malnutrition, etc.) Hyperglycemia without DKA or HHS Considerations ● Most diabetic patients with elevated glucose levels are asymptomatic ● High glucose levels can affect body water balance ● Acute treatment for levels up to 400 usually not needed unless there is a concurrent disease process Evaluation ● Glucose < 400 without other disease processes or symptoms may not need further testing acutely in patient with history of poor control (if vital signs normal and mentation changes or comorbidities absent) ● Tests are directed to disease processes that may be elevating glucose levels ● BMP ● CBC if infection or inflammatory process suspected ● U/A if UTI suspected Discharge criteria ● If new onset obese adult patient with DM without DKA or HHS and glucose < 200 ● Diabetic history with glucose < 400 ● No metabolic acidosis ● No dehydration ● Normal vital signs and no mentation changes Discharge instructions • Hyperglycemia aftercare instructions • Follow up with primary care provider within 1–5 days • Return if patient develops symptoms Consult criteria New onset • New adult onset DM with glucose > 300 • New onset pediatric DM with glucose > 200 mg/dL Diabetic patient with • • • • • • • • • • • Significant comorbid symptoms Metabolic acidosis Vomiting Dehydration Tachycardia Hypotension Relative hypotension SBP < 105 with history of hypertension Orthostatic vital sign changes Progressive renal insufficiency creatinine increase > 0.5 Adult heart rate ≥ 110 Pediatric heart rate 12–15 years ≥ 115 16 years or older ≥ 110 Glucose ≥ 400 in asymptomatic diabetic patient Treatment for Type 2 Adult Diabetes If Desired Obese Monotherapy • Metformin 500 mg PO bid with or after meals 1 week, increase weekly by 500 mg to achieve 1000 mg PO bid Second drug if needed • Micronase 2.5 mg PO qd after breakfast (elderly 1.25 mg PO) Third drug if needed • Avandia 4 mg PO qd OR • Actos 30 mg PO qd Non-obese Monotherapy • Metformin 500 mg PO bid with or after meals 1 week, increase weekly by 500 mg to achieve 1000 mg PO bid OR • Micronase 2.5 mg PO qd after breakfast (elderly 1.25 mg PO) Second drug if needed • Metformin 500 mg PO bid with or after meals 1 week, increase weekly by 500 mg to achieve 1000 mg PO bid OR • Micronase 2.5 mg PO qd after breakfast (elderly 1.25 mg PO) Third drug if needed • Avandia 4 mg PO qd OR • Actos 30 mg PO qd Elderly Monotherapy • Prandin 0.5–4 mg PO up to qid ac (not to exceed 16 mg qd) Monotherapy failure • Consider switch to NPH insulin 10 units SQ bedtime Asians Monotherapy • Avandia 4 mg PO qd OR • Actos 30 mg PO Second drug if needed • Metformin 500 mg PO bid with or after meals 1 week, increase weekly by 500 mg to achieve 1000 mg PO bid Third drug if needed • Micronase 2.5 mg PO qd after breakfast (elderly 1.25 mg PO) Symptomatic patients ● Prandin 0.5–4 mg PO up to qid ac (not to exceed 16 mg qd) or insulin to decrease glucose at start of monotherapy initiation