胸內常用藥品介紹
胸內常用藥品介紹
胸腔內科
Classification
1. Drugs for obstructive lung disease
2. Drugs for infectious disease
3. Drugs for chemotherapy
4. Drugs for symptomatic relief
Drugs for obstructive lung disease
COPD and asthma ( including stable condition and acute exacrbation
Inhaled medication: prefer medicine oral medication
IV and IM medication
GINA (Global Initiative for Asthma)
Guidelines 2002
Intermittent
Mild persistent
Moderate persistent
Severe persistent
Shortacting ß
2 p.r.n
Inhaled Corticosteroid
Sustained-release theophylline
Leukotriene Modifier
Longacting ß
2 agonist
Oral steroid
GOLD guideline (2003)
0: at risk I: mild II: moderate III: severe IV: very severe
Aviodance of risk factors; influenza vaccination
Add short acting bronchodilator when needed
Add regular one or more long acting bronchodilator; Add rehabilitation
Add inhaled steroid
Add long term O2
Inhalation Therapy
液態或固態的粒子懸浮在氣體中便稱
為氣霧(aerosol).經由氣霧粒子攜帶藥
物,水或食鹽水進入呼吸道達到治療的效
果稱為吸入治療.
1.
藥物吸入治療
2.
非藥性( blind )吸入治療(含水或
食鹽水粒子)
Indication and goal of inhaled therapy
1.
呼吸道給藥
2.
稀釋肺部分分泌物與誘發取痰
(hydration of pulmonary secretions and sputum induction)
3. 吸入氣體的濕化
(humidification of inspired gases)
Devices of inhaled therapy
1.
噴嘴式噴霧器 jet nebeulizer
2.
超音波噴霧器 ultrasonic nebeulizer
3.
定量吸入器 metered dose inhaler (MDI)
4.
乾粉吸入器 dry power inhaler (DPI), including rotadisk, turbuhaler, accuhaler & easyhaler
Jet nebeulizer
Spacer as adjuvant therapy
Dry power inhaler (DPI)
Rotadisk
Easyhaler
Accuhaler
Turbuhaler
Easyhaler
Accuhaler ( 胖胖魚 )
Turbuhaler ( 都保 )
Reliever
Short acting b
2 -agonists
(cold color)
Controller
Inhaled corticosteroids
(warm color)
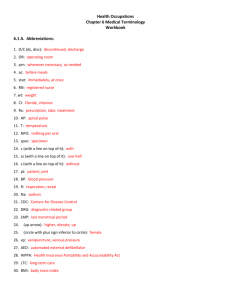
各種器具之優缺點比較
優點
Nebulizer 吸入率8-12%且不需病人配合
可用於人工氣道與呼吸器患者
可作高劑量與持續性治療
不含氟氯化碳不污染環境
MDI 可用於人工氣道與呼吸器患者
方便便宜不易污染
缺點
不經濟藥品易浪費
耗時長易污染
需高流量氣體作動力來源
DPI 吸入率12-16%且不需病人配合
不含氟氯化碳不污染環境
攜帶方便便宜不易污染
吸入率9-12%且須病人高度配合
人工氣道與呼吸器患者吸入率只有4-6%
氟氯化碳會破壞環保
需較高之吸氣流速
無法使用於人工氣道與呼吸器患者
易受濕氣影響
Inhaled Medication
1. b
2 -
agonist
2. Anti-cholinergic agent
3. Steroid
Short acting b
2 agonist
1. Ventolin ( Salbutamol ), nebeulizer , 1 amp
(5mg/2.5 ml), q30 min – q6h prn; MDI 2 puff prn
2. Bricanyl ( Terbutaline hydrochloride ),
Turbuhaler , 200mg/100 dose, 1-2 puff qid prn
Long acting b
2 agonist
Serevent
( Salmeterol xinafoate ),
Accuhaler , 50mg/60
1-2 puff bid
Oxis ( formoterol ),
9 ug / dose.
Turbuhaler 1 puff bid
Anticholinergic Agent
Atrovent
( Ipratropium bromide )
1. MDI , 200 puffs/10 ml,
2-3 puff qid
2. Nebeulizer solution,
0.5mg/2ml/vial,
1 vial qid
Combined β 2 agonist and anticholinergic drug ( Combivent )
Combivent
(Ipratropium + albuterol)
2puff Qid
Inhaled steroid
Pulmicort ( Budesonide )
Turbuhaler : 200ug/200dose/bot,
2-4 puff bid
Nebeulizer : 1000ug/2ml/vial,
0.5 -1 vial bid
Flixotide
( Fluticasone propionate )
Accuhaler
,
250mg/puff/60dose,
1 puff bid
MD I, 50mg/puff/200dose
Combination therapy
(Long acting β 2 agonist + steroid)
Symbicort
( Budesonide + formoterol )
Turbuhaler, 200 puff,
1~2 puff bid
Seretide
(Fluticasone propionate + Salmeterol )
Accuhaler; 1 puff bid
Oral Medication
1. b
2 agonist inolin ( 1# tid-qid); meptin ( 1# bid), bambec 1# qn
2. Xanthine derivates
Phyllocontin 1# bid-tid ( 不可磨碎 ) , theophylline 2# qn or 1# q12h ( 可磨粉,適合
NG feeding 者 )
3. Steroid: prednisolone 0.5-1mg/kg qd
4. Leukotrine modifier:
Accolate 1# bid singulair 1# qd
IM & IV medication
1. Epiphephrine
IM: 0.5 ml sc
IV: 0.5-1 ml slowly IVD
2. Ipradol ( Hexoprenaline Sulfate )
1 amp(5ug/2ml) IM or IV slowly
3. Aminophylline
(must add in saline)
Loading dose: 250 mg x 30 min
250 x 8 hours
6-15 mg/kg qd (serum level 10-20ug/dL)
Drugs for infectious lung disease
1. Community acquired pneumonia( CAP) with and without parapneumonic effusion
2. Hospital acquired pneumonia (HAP)
3. Pulmonary TB
5. Empyema thoracis and lung abscess
6. COPD or asthma with 2nd infection
8. Bronchiectasis with 2nd infection
Community acquired pneumonia
Pathogens: S. pneumoniae; H. influenza; atypical pathogen ( M. pneumoniae,
C. pneumoniae ). Mixed infection, MSSA, and some G(-) bacillus…
Mixed typical and atypical pathogen.
Risks factor or host factor of specific pathogens in pneumonia
Community acquired pneumonia
S. pneumonae : Penicilline, Rocephine or
Vancomycin, fluroquinolone
H. influenza, G(-) bacillus : Unasyn, Augmentin or 2nd and 3rd cephalosporin and fluroquinolone
Atypical pathogens : Erythromicin, klaricid,
Zithromax, tetracycline and fluroquinolone
Mixed infection : Penicillin, Cleocin, Unasyn
MSSA : Cefalosporin, Oxacilline
Hospital acquired pneumonia
Pathogens: G(-) bacillus, P. aeruginosa, MRSA,
VRE, A. baummanii, Legionella..
MRSA : Vancomycin, Targocid
P. aeruginosa : Pipril/Tazocin, Fortum, Cravit,
Ciprofloxacin, Tienam and maxipime
G(-) bacillus : 3rd cephalosporin
Legionella : Erythromycin, Klaricid, Zithromax
A. baummanii : Tienam
Pulmonary TB and TB pleurisy
First line : INH, RIF, EMB, PZA
Secondary line : Fluroquinolone, Aminoglycoside,
PAS, Ethionamide, and Cycloserine
Standard therapy: 6 months
Intensive therapy X 2months: HERZ
Maintain therapy X 4 months HER
If PZA is not used, Keep HER for 9 months
Pulmonary TB and TB pleurisy
Side effect:
INH: hepatitis, peripheral neuropathy
RIF: hepatitis, jaundice, rash
EMB: neuritis
PZA: hepatiits, hyperuricemia, gouty
Steroid & Vitamin B6
Combination therapy:
Rifater: INH 80 + RIF 100 + PZA 250
Rifinah: INH 150 + RIF 30
Thoracis Empyema and
Lung Abscess
1. Treat as pneumonia
2. Adequate drainage
Tube drainage
Decortication
Repeated lung aspiration (abscess)
3. At least 3-4 weeks IV antibiotics treatment and total duration around 6-8 weeks
COPD /c 2nd Infection
Most caused agents
1. H. influenza, G (-) coccobacillus
Tx: Ampicilline/Unasyn, Amoxicilline
/augmentin; 2nd cephalosporin, Macrolidw
2. Moraxella catarrhalis, G (-) diplococcus
Tx: Macrolide, Baktar, Augmentin or
Fluroquinolone, 3 rd generation cephalosporin
3. Streptococcus pneumoniae G(+) diplococcus
Tx: Penicillin, Amoxicilin/ Augmentin,
Ampicilline/ Unasyn
Bronchiectasis with secondary Infection
1. Initial: G(+) coccus + GNB:
Tx as COPD with 2nd infection
2. Later: GNB, especially P.spp
Floroquinolone:
3rd generation cephalosporins
Beta-lactam PCN + aminoglycoside
Tineam + aminoglycoside
Drugs for chemotherapy
1. Small cell lung cancer
( SCLC )
2. Non-small cell lung cancer
( NSCLC )
Small cell lung cancer
First choice
Cisplatin 75 mg/m² x 1 day
VP 16 100 mg/ m² x 3 days every 28 days
Second line
Topotecan 1.5-2.5 mg/m2
Taxol 135 mg/m2 ( 自費 ) every 21 or 28 days
Non small cell lung cancer
First line
1. Gemzar 1000 mg/m² + Cisplatin
100 mg/m² + x I
2. Taxol 135 mg/m² + Cisplatin
75 mg/m² x I
3. Navelbine 25 mg/m² + Cispaltin
75 mg/m² x I
Second line
1. Taxotere 75 mg/m² x I /C or /S Cisplatin
Drugs for symptomatic relief
Insomnia
Cough
Pain
Shortness of breath
Insomnia
看病人
Haldol
Type I receptor : Zopiclone , Zolpidem
Type II receptor : Ativan , Valuim
Antitussive & Expectorants
1. Solution
2. Tablet or capsule
3. Nebular
Solution
1. Brown mixture ( B.M
)
含 opium, 5-10 ml tid – qid
2. Guaifenesin ( Unitussin or G.P
) reduce the visicosity of sputum antihistamine effect (+)
5-10 ml q4h - q6h
3. Fusoco
限小兒科使用 , 成人需自費
Tablet
1. Brown mixture ( B.M
), 1-2# tid - qid
2. Bensau ( Benzonatate ) 1-2# tid - qid
3. Codeine 1# q6h prn
4. Bisco ( Bisolvon ) 1# qid
5. Danzen 1-2 # tid - qid
6. Mucora 1# qid
7. Medicon 1# tid –qid
# 以上藥品不得同時開
立三項 ( 含 ) 以上
Nebulizer
1. Bisolvon aerosol + mucolytic agent
help to expectorate
2. Lidocaine for refractory cough, 2mg/5ml IH
3. Gentamycin
40 mg IH q8h, as immunomodulater
Pain
Acetaminophen
NSAID
Tramadol (50mg) & Tramadol-SR (100mg)
Morphine (10mg PO, IM, IV)
Fentanyl (25μg, 50μg)