Tracheostomies
advertisement

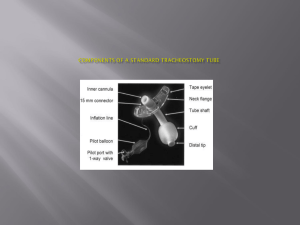
Managing Respiratory Distress and complications post insertion of a Tracheostomy Dr P Chetcuti Consultant Paediatrician and Neonatologist Indications Historically-Upper airways obstruction associated with infections was the most common indication—Diptheria ,polio and HIB vaccines Now most common indication is fixed upper airways obstruction and the requirement for prolonged ventilation secondary to neuromuscular and respiratory problems Changes in last 20 yrs Prematurity increased from 28% to 58% Congenital anomalies increased from 6% to 23% Acquired subglottic stenosis from 2% to 23 % Neuromuscular disease from 9% to 23% Infectious diseases decreased from 50% to 3% Indications for tracheostomy Unsafe or obstructed airway Prolonged mechanical ventilation required Tracheobronchial toilet Alternatives to Tracheostomy Non invasive ventilation-not a 24hr solution,not beneficial if fixed severe obstruction Nasopharyngeal airway Palliative care Indications Upper airways obstruction Subglottic stenosis Tracheomalacia Tracheal stenosis Craniofacial syndrome - PierreRobin,Charge,Treacher Collins Syndrome,Beckwith Wiedemann Craniofacial and laryngeal tumours-cystic hygromas,haemangioma Bilateral vocal cord palsy Obstructive sleep apnoea Laryngeal trauma-burns,fracture Indications Long term ventilation,pulmonary toiletBronchopulmonary Dysplasia,scoliosis,diaphragmatic paralysis Congenital heart disease in association with tracheobronchomalacia,diaphragmatic paralysis and cardiac failure Neurological/neuromuscular diseaseDuchennee muscular dystrophy,spinal muscular atrophy,congenital central hypoventilation syndrome,cerebral palsy,traumatic brain and spine injury,spina bifida Prematurity Increasing no of Tracheostomies in smaller sicker infants-2kg Subglottic stenosis,long term ventilation for bronchopulmonary dysplasia Mortality from tracheostomy related complications high in this group 5-10% More prone to infections The loss of Auto Peep Lose the resistance of nose and larynx Can effect optimal lung ventilationperfusion relationship Makes it more difficult to breath May need supplemental oxygen Age at tracheostomy < 6 months – 56% 6 months to 3 yrs- 32% 3 yrs to 6 yrs – 12% Tube size Too small –difficult to breath hypoventilation may occur especially during sleep Too large a tube can damage airway mucosaulceration and fibrous stenosis Cuffed tubes not used in young children The smaller the tube the more likely the possibility of speech Tubes must be changed with growth-approx every 2 yrs in children under 5 Tube length Too short- will fall out Too long- damage carina or go down r main bronchus At least 2cm from stoma and no closer than 1 to 2 cm from carina Tube care Tube change Fixation Management of secretions Humidification of inspired air Management of stoma-clean,protect and dress Securing the Tube How well the tube is secured is more important than the material- twill tape,velcro and stainless steel beaded metal chains Standard Management Post op CXR 3 days intensive care 1st tube change by doctor who created tracheostomy Tube change weekly suctioning As frequently as required Instillation of boluses of saline ? Minimum morning after waking and pre bedtime Passive Humidifiers Nose,pharynx,larynx and trachea acts as a filter,heater and humidifier of inspired air Not available with Tracheostomy May damage the airway structurally and functionally Ok if ventilated nebulised saline Artificial ‘noses’ humidifiers monitoring Vigilant,well trained and properly equipped care giver Risk-age,size of tracheostomy,degree of airway obstruction,behaviour of child,underlying pathology,the presence of other underlying medical conditions and the social environment No monitoring devices are ideal Monitoring in hospital Cardiorespiratory monitoring Oximetry Early complications Pneumomediastinum and pneumothorax Haemorhage Accidental decannulation-reduced with stay sutures-small curved artery clamp should be available at bedside plus 2 spare tracheostomy tubes(one smaller) Tube blockage-frequent suctioning required to prevent Subcutaneous emphysema-avoided by using appropriate sized tube and not making wound too tight Intermediate Local infection-can produce excessive granulation tissue-can make it difficult to reinsert tube Late complications Difficult decannulation Psychological dependance Tracheal granulomas-due to trauma at distal end or excessive suctioning +/infection Accidental decannulation-mortality 2% Suprastomal collapse and tracheal stenosis Late complications Persistent tracheocutaneous fistula-1942% Effect on speech and language-age at time and length of time Erosion into the innominate artery Tracheo-oesophageal fistula Failure of decannulation Peristomal pathologygranulations,suprastomal collapse,stomal tracheomalacia,stenosis Granulations-surgical removal,laser,?potassium titanyl phosphate Underlying pathology not adequately resolved Rigid or flexible bronchoscopy every 6 to 12 months Causes of death associated with tracheostomy Accidental decannulation Tube obstruction-increasing likely in small infants—narrrow airay,narrow tubes,copious viscid secretions(bronchopulmonary dysplasia) 11% mortality under 6 months of age(0.5 to 3%) Tube Blockage Obstructive breathing Cant clear secretions on suctioning Urgent tube change required Signs of Chest Infection Thick discoloured secretions +/- Unwell off feeds drowsy +/- pyrexia +/- Tachypnoeic/chest wall recession +/- CXR changes Secretions for viruses bacteria Tracheostomies-infection Increased risk of lower respiratory infections Treat with oral or gastric antibiotics Infections around tracheostomy-good wound care +/- antibiotics—may leed onto mediastinitis if not treated optimally Colonisation commonpseudomonas,MRSA and staphyloccus aureus,candida Other respiratory management ? Salbutamol spacer/nebuliser ? Ipratropium spacer/nebuliser ? Steroids—spacer/nebulise/oral IV antibioics ? Montelukast ? nebulised hypertonic saline ? Dnase ? Nebulised antibiotics Speaking valves Various different types Attaches to the open end of tracheostomy Valves close on expiration directing air into the upper airway and across the larynx May be used in infants Make it more difficult to breath Speaking valves-contraindications Presence of severe obstruction A laryngectomy With cuffed tubes In the presence of excessive secretions With gross aspiration With bilateral adductor cord palsy Challenge of giving oxygen Side tubing Masks Cpap Do not rely on oxygen sats as an indicator of a blocked tube Oral Feeding May deteriorate temporarily or permanently after tracheostomy Depends on pre tracheostomy feeding Difficult in prems and ex prems Nasogastric feeds and Gastrostomies sometimes required Milk in tracheal secretions is not good Speech development Other factors-prolonged hospitalisation,neurological problems,chronic middle ear problems, lack of normal feeding experiences, lack of muscle strength Do better if decannulated early Speech therapy Speaking valves Sign language Home care Tube –change,fixation,suctioning-shallow and deep Saline instillation Suction equipment Clean technique Humidification Application of drugs Stoma care Monitoring-continuous presence of a competent carer monitoring device ? Feeding Bathing Clothing-not fluffy,dressing and undressing must not be over the head Home care Adaptations –electrical sockets,storage space,space, Transportation Safety-smoke,pets,household sprays Extra support Time in hospital day and night prior to discharge is required Lots of support required Organisation of services Dedicated Nurse specialists Specialist multidisciplinary clinics Children should not be transferred to hospitals if nurses not adequately trained in smaller hospitals Resources ‘Stretched’in larger hospitals