INDICATIONS FOR CHANGING TRACHEOSTOMY TUBE
advertisement

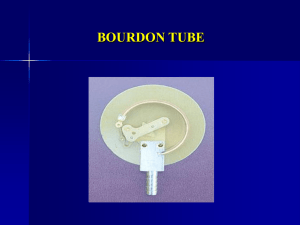
TRACHEOSTOMY CARE Rosie Ratcliffe (Previous Macmillan Head and Neck Clinical Nurse Specialist) Amended 2012 Aims To provide basis awareness of caring for patients with tracheostomy tubes To understand the safety implications when dealing with tracheostomies To understand complications and emergency procedures with tracheostomy tubes What is a Tracheostomy? A tracheostomy is a surgical procedure that is usually performed under a GA or LA (tracheotomy). It is an incision into the trachea (windpipe) that forms a temporary or permanent opening called a stoma A tube is inserted through the opening to facilitate breathing, protection from aspiration in cases of swallowing impairment and facilitate clearance of secretions Reasons for a Tracheostomy Airway obstruction e.g. Upper airway tumours Lower airways toilet Neurological disease e.g. MND Vocal Cord Paralysis Laryngeal injury or spasms Severe neck / mouth injuries Airway burns from inhalation smoke/steam Anaphylaxis Types of Tracheostomy Tubes Double lumen tubes – consist of inner and outer tubes to aid clearance of secretions without changing the complete tube. Tracoetwist, Tracoecomfort, Shilleys Fenestrated tubes – these are double lumen with holes built into the shaft to allow air to flow through the vocal cords to facilitate speaking Both these tubes come either non-cuffed or cuffed Cuffed tubes - low pressure air filled cuff at the distal end of the tube allows sealing of the airway used to prevent aspiration and facilitate ventilation Cuffed tubes Seal the airway to facilitate the delivery of positive ventilation Prevent airflow through larynx Protect the airway Prevent risk of aspiration External pilot balloons which indicate when the cuff is inflated or deflated The cuff may impair swallowing due to pressure on the oesophagus Un-cuffed tubes Maintain airway patency Do not protect from aspiration Enable voice around the tube May be used to wean Used for long term tracheostomy patients Not commonly seen in the acute setting Cuff pressures Cuff pressure should be maintained between 15 – 22mmHg Check pressure by using manometers – every shift, minimum of twice in 24 hours Minimal occlusion pressures / minimal leak texhnique (auscultation around suprasternal notch) not recommended due to risk of silent aspiration Voice Syringe Common complications Tracheostomy complications are usually divided into 3 categories Intra-operative Early post-operative Late post-operative Intra-operative Bleeding Tube malpostion Tracheal / trache-oesophageal laceration Recurrent laryngeal nerve damage Pneumothorax Early post-operative Bleeding Tube blockage Infection Subcutaneous surgical emphysema Tube malpostion Displacement Late post-operative Granuloma (growth of inflammatory tissue caused by irritation) Tracheal stenosis (abnormal narrowing of trachea e.g. from tracheal tumour) Tracheomalacia (flaccidity of tracheal cartilage causing tracheal collapse e.g. from fistula) Trachoesophageal fistula Mucosal ulceration Main life-threatening complications and their management - Bleeding Bleeding – this is the most common complication of a tracheostomy. It may occur early or late. Minor- settles with conservative management Major- requiring blood transfusion, surgical exploration / other intervention Management depends on the context in which the bleeding occurs Palliative management: Dark green towels, crisis medication, psychological support, suction, external pressure to bleeding site, communication to patient / family debated. Priority - STAY WITH PATIENT Tube blockage Tracheostomy tubes can become blocked with thick tracheal secretions, blood or foreign bodies. Presentation may be increasing respiratory distress over a few hours or more rapid deterioration This can be LIFE THREATENING if not rapidly resolved Prevention - adequate humidification, regular inner tube changes, suction Displaced trachesotomy tubes Tubes can become displaced through a loose or inadequately positioned neck tape, excessive movement of the patient, patient agitation or pulling of equipment that is attached to the tracheostomy tube. A dislodged tube is more dangerous than a completely removed tube Prevention - regular checks of neck tape, ensure equipment is attached safely, manage agitation, regular observation of patient. Suctioning Suctioning can be both uncomfortable and distressing for the patient, therefore where possible patients should be encouraged to expectorate their own secretions Patients individual needs need to be assessed frequently Indications for suctioning - unable to expectorate, blockage in tracheostomy tube Suctioning Complications Hypoxia Bradycardia Tracheal mucosal damage Bleeding Infection Types of humidification Heat and Moisture Exchanger (HME) Thermovent –T, Inter-surgical HME common in acute settings Trachi-naze filters, Buchanan bibs common in long term settings Water humidifiers - Fischer-Paykel (heated) Respiflow (cool) Saline nebulisers Trachi-spray NORMAL MECHANISM OF HUMIDIFICATION 20°C 50% 34°C 75% Temp 37°C, Rel. Humidity 100% 5cm below carina Tube changes Tracheostomy tubes should be changed every 28 days as per the European Economic Community Directive (1993) The first tube change should be carried out by a medical practitioner with appropriate, advanced airway skills Health professionals who have undergone training and confident / competent INDICATIONS FOR CHANGING TRACHEOSTOMY TUBE: Elective: Monthly Assess stoma/ trachea and granulation tissue at stoma site and / or fenestration Facilitate weaning Speech production Patient comfort Emergency Blocked tube Misplaced or displaced tube Cuff failure Faulty tube Aspiration Hypoxia Anxiety/Discomfort Stoma care Review stoma each shift Assess stoma Clean with NaCl and dry carefully Use barrier cream to protect skin Apply trachi dressing under tube Change neck tapes at least weekly Ensure neck tapes are secure allow 2 fingers to fit between the tapes and neck Communication The impact of the loss of normal voice following a tracheostomy should not be under estimated Loss of voice occurs because no air is passing over the vocal cords Communication facilitates- expression of feeling, reassurance, patients needs, advice, counselling, social interaction, information giving Alternative methods of Communication Non-verbal Lip reading Coded eye blinking Hand gestures Alphabet board / Picture borad Light writer Cuff deflation / fenestrated tubes Intermittent finger occlusion Speaking valves SPEECH Teaching patient to live with Tracheostomy Need lots of reassurance and advice Involve patient in stoma care from an early stage, changing inner tube frequently Involve SALT with swallowing and speaking Show patient how to clean around stoma and encourage this on a daily basis Advice re: looking after skin around stoma site Altered body image TROUBLE SHOOTER deflation Leak due to deflation cuff. Partial withdrawal Ulceration into oesophagus Leak due to deflation and surgical emphysema Obstruction due to herniation of cuff over end of tube. Obstruction due to kinking Misplacement into pre-tracheal tissues. Blockage by secretions Dilation of trachea by over inflated cuff. Summary Each shift always check the tracheostomy tube is patent Know what type / size of tube is in place Know patients normal observations if appropriate Know if the cuff is inflated / deflated Know emergency procedures Refer to protocol Always know the patients resuscitation status Any questions?