Quiz Terms #2 - WordPress.com
advertisement

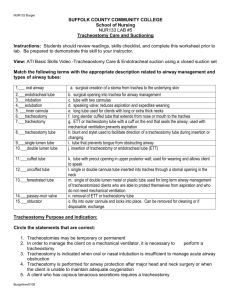
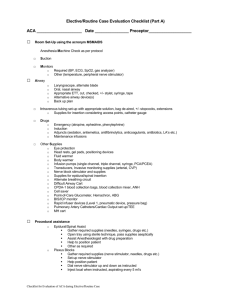
Tracheostomy Tracheotomy is the surgical incision into the trachea for the purpose of establishing an airway. Tracheostomy is the stoma, or opening, that results from a tracheotomy. May be temporary or permanent. Nursing Assessment: Auscultation of the lungs Monitor o2 sats Assess for any increase in the amounts of blood in the sputum SC emphysema in the neck Respiratory distress Patency of the tracheostomy tubing itself. Tracheostomy Accidental Decannulation Removal of the tub Typically occurs with downsizing the tube and/or capping the trach tube to block air from moving through it and allowing the pt to breathe through the normal respiratory structures. Artificial airway requires humidification to the airway because the normal upper airway passages that humidify sections are bypassed. Encourage pt. to do C&DB Suction may be necessary to assist in clearing secretions IN ALL CASES OF BLEEDING, nurse must suction the tracheostomy tube to maintain patency of the patient’s airway and inflate the cuff if one is present. Nurse must call for help, as this is an emergent situation. Ensuring that the inner cannula is changed routinely to prevent occlusion is an important component of the nursing care. Cleaning trach site involves cleaning around the tube with half-strength hydrogen peroxide on cotton swabs and rinsing with normal saline. Keep faceplate flush with the skin of the neck. Check the ties frequently, and change them if become soiled or wet. Duo-Derm or a stoma wafer can be used to protect the skin. The nurse should teach the pt. to occlude the end of the trach tube with a finger in order to speak on exhalation. Monitor patient’s oxygen and respiratory status. Take not of any changes in patient’s behavior. (Restlessness, agitation, or changes in LOC.) If ^^ occur, remove inner cannula and start suction. If cannula cannot be inserted, tube may have been dislodged. Remain with the patient and position pt. with Head up and slightly extended. Pt may need to be ventilated with a resuscitation bag until the airway is replaced. It is critical for the nurse to teach the patient how to uncap or remove the cap of the tube. Care issues for patients with tracheostomy Prevention of tissue damage Cuff pressure can cause mucosal ischemia. Minimal leak technique and occlusive technique. Check cuff pressure often. Prevent tube friction and movement. Prevent and treat malnutrition, hemodynamic instability, or hypoxia. Discharge priorities for patients with a tracheostomy Safety with an artificial airway is the priority for teaching Teaching patient: o Suctioning o Saline instillation o Wound care o Inner cannula care o Emergency measures Assess the patients ability to read and write prior to surgery and establish a suitable form of communication. Must demonstrate safe care before discharge Head and Neck Cancer Cells change from the normal division to altered cells that grow along tissue planes and into adjacent structures. Obstructive Sleep Apnea Patient stops breathing for more than 10 seconds with five or more episodes per hour Caused by physical obstruction from tissues in the upper airway. Air cannot flow in or out of the person’s mouth despite efforts to breathe. Gas exchange (02, HR, pallor, cyanosis, cough, accessory muscles, lung sounds, LOC, ABG) Nasal drainage for presence of CSF Skin integrity (Color, blanching, odor, bleeding, wound assessment) Nutrition (Bowels, lungs, residual volume pain management Change of sleep position (side lying) Weight loss Positive-pressure ventilation o Continuous PAP (CPAP)- continuous constant o Bilevel pap (BPAP)- titration in inspiration and expiration pressures separately o Auto-titrating PAP (APAP)- pressures that are more patient driven, depending on airflow, circuit pressure, or snoring Noctural dialysis (if kidney failure) Avoid use of tobacco, alcohol, and sleeping pills. Dental device that moves tongue forward Evidenced by the paradoxical motion of the abdomen and rib cage with respiratory effort Laryngectomy Removal of the larynx Necessitates a permanent tracheal artificial airway Explain to the patient and family of all the risks and benefits of each form of treatment. Support patient in whatever decision is made, even if it might not seem the best choice for complete for complete removal of the disease. NG feeding tub placed intraoperatively because the internal incision in the pharynx takes 5-7 days post Laryngectomy. Before the patient resumes an oral diet, a barium swallow is completed to evaluate the internal suture lines in the pharynx, thereby ensuring that the suture lines are intact and there is no leak of barium through the incisions. Be patient with the patient with a tracheotomy or someone on voice rest. Airway maintenance, pain management, nutrition, and wound healing. Drain assessment and care Carotid artery exposure assessment and management. POWERPOINT Airway maintenance and ventilation Wound Care - Reconstructive Flaps, Graphs Bleeding Pain management Nutrition Speech and language rehabilitation Myocutaneous flap Flap composed of muscle and skin, used to reconstruct the defect caused by the tumor resection. Chyle Leak Carotid artery expose and potential rupture A disruption in the lymph system that causes lymphatic fluid to leak from the thoracic duct on the left side and the lymphatic duct on the right side. Can occur with a patient who has problems with wound healing, fistula formation, poor nutrition, and/or history of radiation therapy to the When the nurse assesses a reconstruction flap, myocutaneous, or free, it should be pink and warm with brisk cap refill (<2sec) Tracheostomy and cupola ties (ties that secure the oxygen to the trach mask in place) should be positioned away from the graft to prevent pressure on the area. The head position should be maintained straight or toward the operative side to prevent pressure or tension on the flap. HOB elevated at least 30degrees to facilitate drainage of the fluid and to prevent edema of the head and neck. Nurse should report this condition to the healthcare provider immediately because it can result in serious fluid and electrolyte imblances. Monitor pt. H/H and careful assess vital signs if bleeding occurs. Report decreased in H/H and/or any increase in the pulse rate and decrease in BP to the surgeon. Carotid tray at bedside Four packages of fluffs at bedside Dual-suction machines with large oral suction at bedside area. Cystic Fibrosis (CF) Atelectasis An autosomal recessive hereditary disease of the exocrine glands that primarily affects the respiratory and GI systems. Collapsed alveoli Portable suction on unit for transport One-liter LR solution at bedside with connecting tubing Two large bore IVs at all times Type and antibody screen every 40 hours or per hospital protocol. Two units heparin at bedside Post op wound care: o Saline soaked dressings (wet-wet every 2 hours) o When stable and healing, advance every 2 hours while awake and every 4 hours at night, with wetting of the dressing with normal saline every 2 hours o Frequent observation of patient for “herald” bleed (premature bleed), dry or dark area of artery or aneurysm formation o Call the house officer or surgeon immediately if any of the above occurs o Assess for a higher level of care if other compounding problems are present such as infection. o Alert the OR and blood bank that patient is on carotid precautions Medication as ordered Providing oxygen therapy Instructing the patient and family on nutrition and exercise. Home care instructions o Postural drainage techniques o Aerosol-nebulization therapy o Breathing retraining o C&DB C&DB HOB up to 30-45 degrees Administer oxygen as ordered or by hospital protocol Instruct patient to do “huff cough” Encourage use of incentive spirometer