Cardiac Stimulants and Depressants
advertisement

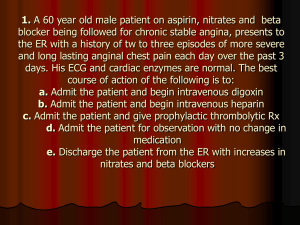
Antiarrhythmic Agents: Cardiac Stimulants and Depressants The Heart Four-chambered organ located in the upper left thoracic cavity Purpose Pumps the blood around the body so that oxygen and nutrients can be distributed to all areas of the body Maintains the blood pressure at an acceptable level Generates and conducts electrical impulses Heart rate is controlled by the autonomic nervous system 17 - 2 The Heart Main pacemakers of heart: Sinoatrial node: 60-100 bpm; primary pacemaker Atrioventricular node: Connects atria and ventricles; 40-60 bpm Bundle of His and Purkinje fibers: carry electrical impulses from AV node to complete ventricle rate pacing; 1540 bpm 17 - 3 Cardiac medications Increase /decrease the force of the myocardial contraction Increase / decrease the heart rate Increase / decrease the conduction of electrical impulses through the myocardium 17 - 4 Congestive Heart Failure (CHF) Cardiac glycosides -Digoxin -Treat arrhythmias 17 - 5 Cardiac Glycosides Derived from natural sources; treatment for heart failure: cardiac distention-inability to pump the full blood volume cardiac hypertrophy-prolonged stretching sodium and water retention-decreased renal blood flow Results in weight gain, edema, shortness of breath, and pulmonary congestion 17 - 6 Digoxin Decreases electrical conduction Negative Dromatotropic Effect Increases time spent in diastole Increases the force of the myocardial contraction Positive inotropic action End result: slows and strengthens contractions 17 - 7 Digoxin: Dose Considerations Duration of action Method of administration Other Physical size of the client Other medications Renal or hepatic function Advanced age Presence of other illnesses 17 - 8 Digoxin Low therapeutic index Toxicity can be life-threatening; occurs in 10-20% of patients Many drug-drug, drug herbal interactions Routine monitoring of serum potassium and digoxin levels 17 - 9 Digoxin: Adverse Effects Gastrointestinal effects Nausea and vomiting Anorexia Diarrhea Cardiac effects Cardiac arrhythmias Neurological effects 17 - 10 Cardiac Glycoside Toxicity Predispose to cardiac glycoside toxicity Hypokalemia Renal impairment Rapid IV administration 17 - 11 Cardiac Glycoside Toxicity Treatment Stop the drug Physical assessment Check potassium level Administer if needed Monitor heart rate Administer antiarrhythmics 17 - 12 Nursing Considerations Apical pulse for 1 minute. Hold if HR < 60 bpm Report changes in heart rhythm Assess for symptoms of toxicity Monitor digoxin blood levels Monitor for drug-drug and drug-herbal interactions Educate : signs of toxicity and how to monitor pulse rate . 17 - 13 Antiarrhythmic and Antidysrhythmic Drugs Grouped together according to their similar actions Work three ways: Decrease automaticity of cardiac tissues in the ectopic sites Alter rate of conduction Alter refractory period of cardiac muscle between consecutive contractions 17 - 14 Antiarrythmic Agents Dependent on: type of dysrhythmia presence of other conditions safety of the drug onset and/or duration of drug action Administered IV until patient stabilized, then oral agents given Arranged into classes 17 - 15 Antidysrhythmic Medications Class 1 (1A, 1B, 1C): decrease the influx of sodium ions, stabilizing membranes Class 2: decrease contractility, B/P, AV node conduction Class 3: Prolong action potential, refractory period Class 4: Decrease myocardial contractility, 02 demand 17 - 16 Antidysrhythmics Quinidine gluconate – Class 1 Lidocaine – Class 1B Dilantin – Class 1B Propranolol – Class 2 Verapamil HCL – Class 4 Digoxin – Class 4 17 - 17 Adverse Effects GI upset Cardiovascular disorders Hypersensitivity Hypotension Bradycardia Lightheadedness 17 - 18 Nursing Considerations Take patients apical pulse for one minute Record rate and rhythm of the heartbeat Assess allergies Monitor blood pressure Patient should be supine when administering IV agents . 17 - 19 Beta-adrenergic Blocking Agents Block the hormone epinephrine Inhibit beta and beta2 sympathetic receptors Reduce heart rate Reduces contractility Slow electrical conduction Decrease the blood pressure 17 - 20 Beta-Adrenergic Blocking Agents Adverse effects Cause bronchoconstriction Can cause heart failure Examples: propranolol (Inderal), esmolol, bretylium tosylate (Bretylol) 17 - 21 Calcium Channel Antagonists Reduce the influx of calcium into the cell: Prevention of reversal of spasms of the coronary blood vessels Coronary artery dilation Reduction of myocardial oxygen consumption Example: Verapamil . 17 - 22 Adverse Effects Vasodilation may cause: Hypotension Edema Dizziness Headache Slower myocardial conduction may cause: Bradycardia Heart failure Other effects: Constipation, diarrhea, nausea, fatigue 17 - 23 Patient Education Ensure understanding of drug regime Review signs to report to their health care provider Instruct patient how to take their pulse Remind them of the importance for proper follow-up Encourage questions 17 - 24