Drugs for the Treatment of Gastrointestinal Disorders
advertisement

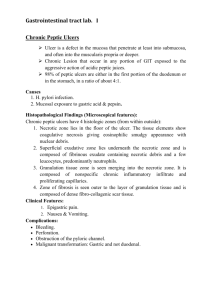
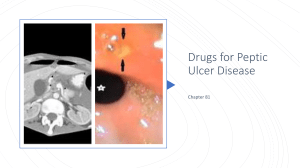
Drugs to Treat Gastrointestinal Disorders Clinical Indication Prevention or management of gastric or duodenal ulcers Management of gastroesophageal reflux disease (GERD) Digestion and Acid Secretion Stomach secretes hydrochloric acid (HCl) in • • • • anticipation of eating (psychostimulation) response to distension from food mass to break-up food prior to transfer to the intestines during sleep to reduce bacterial growth Duodenum secretes • • an inhibitory enzyme that stops gastric acid secretion mucus to lubricate the intestinal lining and avoid autodigestion Acid secretion is mediated by Hormones, neurotransmitters, and histamine Production of Ulcers Ulcers, open sores in the mucosal lining, occur in the stomach and intestines when acid and pepsin activity is overactive from emotional stimulation or alcohol drugs inhibit mucus production(ulcerogenic) predisposing factors are present such as smoking, alcohol, vagal stimulation presence of Helicobacter pylori bacteria Symptoms of Ulcers • • • • • Pain due to acid stimulation of nerve endings Nausea Vomiting Loss of appetite Blood loss through erosion of the mucosal lining • Anemia from chronic blood loss • Hypotension and shock from blood loss Treatment of Ulcers Reduce gastric acid secretion (antisecretory) antihistamines (H2-receptor antagonists) prostaglandins proton pump inhibitors anticholinergic drugs Reduce gastric acid irritation on mucosal lining neutralize gastric acid (antacids) Protective barrier/coat mucosal lining sucralfate Antibiotics H2-Receptor Antagonists Histamine receptors on the parietal cells mediate the secretion of gastric acid and pepsin H2-receptors are different than H1-receptors that mediate hypersensitivity and allergic reactions Cimetidine, ranitidine, famotidine, nizatidine These drugs differ in their potency and ability to affect liver microsomal enzymes Adverse Effects of H2- Antagonists • • • • • Headache Constipation Reversable mental confusion Disorientation in elderly Elevated serum liver enzymes (AST, ALT) Prostaglandins Prostaglandin receptors mediate bicarbonate production and mucus secretion Misoprostol Inhibits the ulcerogenic effect of chronic high dose NSAIDs Adverse effects include diarrhea headache nausea flatulence Should never be given during pregnancy or if the woman is considering becoming pregnant due to abortifacient activity Proton Pump Inhibitors Proton pumps mediate the exchange of potassium ions (K+) for hydrogen ions (H+) within parietal cells Omeprazole, lansoprasole Used for acute treatment of gastric ulcers and GERD, and long-term treatment of hypersecretory conditions, in combination with antibiotics for ulcer healing Adverse effects include headache, nausea, diarrhea, abdominal pain, constipation Antacids Sodium bicarbonate, magnesium hydroxide, aluminum hydroxide, calcium carbonate • Neutralize gastric acid • Most are not absorbed into the circulation • Small amounts of the ions (aluminum, magnesium, and calcium) may be absorbed • Short duration of action • Cause acid rebound with chronic use Adverse effects Constipation Sodium bicarbonate- fluid retention, increased blood pressure GERD: Gastric Stimulants Induce contractions within the upper GI tract • prevent reflux of acid into the esophagus • promote gastric emptying • move damaging substances away from the esophagus • Stimulate cholinergic receptors selectively within the GI tract metoclopramide, cisapride Adverse effects • • • • • • GI Stimulants Metaclopramide Cisapride Diarrhea Dry mouth Headache Constipation Dizziness Abdominal pain Restlessness Rhinitis Sinus tachycardia Sinus tachycardia Hypersensitivity Hypersensitivity Contraindications Cisapride combination with antifungal and antibacterial drugs leads to cardiotoxic blood levels of cisapride Patients with seizures or extrapyramidal symptoms or active GI hemorrhage or perforation Anticholinergic Antispasmodic Drugs Irritable Bowel Syndrome (IBS) Antispasmodic drugs relax intestinal smooth muscle Dicyclomine, oxyphencyclimine Anticholinergic drugs Anisotropine, clindinium bromide, isopropamide, methscopolamine, propanthelene Special considerations: Patients with glaucoma, tachyarrhythmias or bladder Obstructions Contraindications Patients with narrow angle glaucoma, bowel obstruction Vomiting (Emesis) Mechanism Vomiting occurs by CNS stimulation of the • chemoreceptor trigger zone (CTZ) and • vomiting center (VC) Stimulants include • toxins, uremia • electrolyte imbalance • hormonal imbalance in pregnancy • radiation & chemotherapy • intense smell, memory, sight, motion Antiemetics Drugs that block vomiting are known as antiemetics and include • Antihistamines (H1-antagonists) • Metoclopramide • Anticholinergics • Phenothiazines • Serotonin antagonists (ondansetron, granisetron) • Phosphorylated carbohydrate (sugar) solution Motility Agents Clinical Indication Antidiarrheal drugs Prevent or interrupt increased intestinal motility causing diarrhea Laxatives Prevent or interrupt decreased intestinal activity producing constipation Bowel Function Increase in intestinal motility produces a watery stool (diarrhea) through • Stimulation of parasympathetic nervous system • Irritation of mucosal lining (drugs or infection) • Antibiotics that create an imbalance in normal intestinal flora Decrease in intestinal motility produces compacted stool difficult to expel (constipation) through • Stimulation of the sympathetic nervous system especially through anxiety and emotional triggers • Daily diet inadequate in fiber and fluid intake • Habitually ignoring the defecation reflex Antidiarrheal Drugs Adsorbents Bind irritating substances for excretion bismuth subsalicylate, kaolin and pectin, attapulgite Anticholinergics Inhibit parasympathetic nervous system, slow intestinal motility facilitate water absorption atropine, belladonna, scopolamine Opiates and Narcotic derivatives Are anticholinergic and induce muscle spasms (spasmogenic) difenoxin, diphenoxylate, loperamide, paregoric Adverse Effects & Contraindication Adverse effects • Most frequent adverse effect is constipation • Diphenoxylate may be absorbed and produce dizziness, blurred vision, nausea, and rash Contraindication • Anticholinergic drugs should not be used in patients with glaucoma because intraocular pressure may increase Laxatives and Cathartics Emollients Allow water to penetrate the fecal mass mineral oil Osmotic (saline) laxatives Contain sodium ions that attract water into the feces sodium phosphate salts, magnesium citrate, PEG-ES Stimulants Irritate the intestinal lining and promote histamine release increasing intestinal motility bisacodyl, castor oil, senna preparations Stool softeners docusate sodium, docusate calcium, docusate potassium Swelling agents Natural fibers or grains that soak up water and expand bran, prunes, psyllium hydrophillic Adverse Effects Laxatives that contain sodium, phosphate, or magnesium will be absorbed and excreted through the kidneys. The absorbed ion load may produce • CNS depression • Cardiac arrhythmias • Edema in renal impaired patients • Depressed muscle function Osmotic laxatives can cause a large loss of water leading to dehydration, especially in elderly patients