Drugs Used in Gastrointestinal Disorders
advertisement

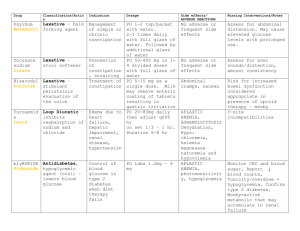
1 Drugs Used in Gastrointestinal Disorders Gastric A & P First, some background physiology…. There are 3 cells of the gastric gland: 1. Chief Secretes pepsinogen pepsin Breaks down proteins in the diet 2. Mucoid Secretes mucus Provides a protective mucous coat to protect stomach from digestion of itself from hydrochloric acid (HCl) 3. Parietal Secretes hydrochloric acid Keeps the pH of the stomach between 1 and 4 so as to properly digest food The wall of the parietal cell has 3 types of receptors: acetylcholine, histamine, and gastrin. When any one of these receptors is occupied, the parietal cell will produce and secrete HCl The receptors can also be blocked: Atropine (an anticholinergic) blocks acetylcholine from binding with the acetylcholine receptor Histamine-2 (H-2) blockers block histamine from the mast cell from binding with the histamine receptor When any of these receptors are bound, the parietal cell is stimulated. The cell must now produce HCl, but needs hydrogen ions (H+ ions) to do so. These H+ ions are produced by the proton pump (H+/K+ ATPase pump) of the cell. The proton pump needs energy to function. So: Energy activates the H+/K+ ATPase system (proton pump) proton pump produces H+ ions needed for the production of HCl HCl is secreted into the stomach Proton pump inhibitors bind to the H+/K+ ATPase pump and irreversibly inhibit this enzyme, resulting in a total inhibition of H+ ion secretion from the parietal cells. The most common impairment is hyperacidity, or the overproduction of acid. GERD = gastroesophageal reflux disease The most harmful is peptic ulcer disease. Theory of how formed: aggressive (acid + pepsin) and protective (mucosal layer) 2 Anti-peptic agents Antacids - Cheapest - Mainstay of antiulcer therapy until the 1970s - Neutralize acid, stimulate mucus and bicarbonate secretion, improve blood flow to area increase protective layer - Problems - Mg diarrhea, Al constipation - Al, Mg, Ca renal patients unable to eliminate - Use caution if the antacid is high in sodium content in patients with CHF, HTN, sodium restrictions, and other cardiac diseases - Best acid neutralizing capacity AND lowest sodium content: Riopan Plus (Al-Mg) and Maalox TC (Mg, Al, simethicone) - There are many drug interactions with antacids because of the effect on absorption of the medication that is given concurrently with the antacid…check for interactions before ordering the medication. - Best not to administer other meds within 1-2 hours after an antacid. - Especially important to separate by 2 hours: dig, iron, INH, quinolones, tetracyclines - Antacids may result in premature dissolving of the enteric coating of meds, resulting in stomach upset. - Increasing the pH of the stomach with an antacid will cause drugs that are acid salts (HCl salts) to be more ionized and less absorbed and drugs that are basic salts (sulfate salts) to be less ionized and more readily absorbed into the bloodstream. - The same alteration in absorption in the stomach will affect excretion of basic and acidic drugs in the urine because the urinary pH will be elevated and acidic drugs will be more ionized, less absorbed, and more excreted. H2 Blockers/Antagonists - Began being used in the 1970’s - Bind to and block histamine receptors located on parietal cells - This blockade renders the parietal cells less responsive to stimuli and thus acid secretion. - Up to 90% inhibition can be achieved with these agents (dose-related) - Indications - Ulcer (gastric, duodenal) - GERD - Upper GI bleeding - Hypersecretory conditions (Zollinger-Ellison syndrome = non-insulin-secreting pancreatic tumor; releases large amount of gastrin) - Examples (and their equipotent dosages) - Cimetidine (Tagamet) 1600 mg. - Ranitidine (Zantac) 300 mg. - Nizatidine (Axid) 300 mg. - Famotidine (Pepcid) 40 mg. 3 - - - All are equally effective in healing ulcers; need to look at pharmacokinetics and adverse effects - Tagamet = shortest ½ life - Pepcid = longest ½ life - Caution with renal /hepatic dysfunction Problem with Tagamet: inhibits the hepatic enzyme (cytochrome P-450 system) metabolism of the following drugs, thereby increasing their levels and effects: - Theophylline - Phenytoin - Oral anticoagulants - Propranolol - Procainamide - Quinidine - Lidocaine - Calcium channel blockers Adverse effects of H2 blockers (worse with patients with multiple illnesses, elderly, those with hepatic or renal dysfunction) - CNS effects (headache, lethargy, confusion, depression, hallucinations (<1%) - Endocrine (impotence, increased prolactin, gynecomastia) - GI (diarrhea, abdominal cramps, jaundice, increased LFTs) - GU (increased BUN, creatinine) - Hematopoietic (agranulocytosis, thrombocytopenia, neutropenia, aplastic anemia) - Integumentary (urticaria, rash, alopecia, sweating, flushing exfoliative dermatitis) Proton Pump Inhibitors - More effective than H2 blockers - More expensive than H2 blockers - Block the final step in the acid production pathway - Blocks all acid secretion - Examples: - omeprazole (Prilosec) 10, 20, 40 mg (also available OTC and generic) - lansoprazole (Prevacid) 15, 30 mg - rabeprazole (AcipHex) 20 mg - pantoprazole (Protonix) 20, 40 mg - esomeprazole (Nexium) 20, 40 mg - dexlansoprazole (Dexilant, Kapidex) 30, 60 mg - omeprazole/sodium bicarbonate (Zegerid) 20 mg/1.1 g; 40 mg/1.1 g - Adverse effects - CNS (headache, dizziness) - GI (diarrhea, abdominal pain, N, V, anorexia) - GU (proteinuria, hematuria, glycosuria) - Hematopoietic (pancytopenia, thrombocytopenia, neutropenia, leukocytosis, anemia) - Integumentary (rash, dry skin, urticaria, pruritis, alopecia) - Respiratory (URI, cough) - Other (back pain, fever, fatigue) 4 - Used for treatment of H. pylori - Example: 2 weeks of Prilosec 40 mg once daily plus Biaxin 500 mg 3X/day; follow with 2 week course of Prilosec 20 mg once daily - Example: PrevPac: 1 dose bid X 14 days (1 dose = 1 tab of lansoprazole 30 mg [Prevacid], 2 tabs amoxiciliin 500 mg, and 1 tab clarithromycin 500 mg [Biaxin]) Sucralfate (Carafate) - A cytoprotective agent for stress ulcerations and PUD (peptic ulcer disease) - Binds to exposed proteins of ulcers and thus limits pepsin’s proteolytic action - Made of sucrose, Al, sulfate - Drug effects - Sulfate anions bind to positively charged tissue proteins that are exposed at the tissue surface of an ulcer or an erosion - As a weak base, it buffers the acidic pH of the stomach - Binds and concentrates epidermal growth factor (EGF), which accelerates the healing process - Simulates gastric mucosal prostaglandin E2 synthesis - The aluminum salt stimulates the secretion of mucus and bicarbonate from the cells of the stomach to counteract the actions of HCl - Side effect: constipation - Renal patients may have problems with Al - Good drug for long-term use - Separate drugs by 2 hours; ciprofloxin should not be used at all Misoprostol (Cytotec) - A synthetic prostaglandin analog - Inhibits gastric acid secretion, enhances local production of mucus or bicarbonate - Also helps maintain mucosal blood flow - Used in drug induced PUD (from NSAIDs) or for gastric ulcer prophylaxis during NSAID therapy [Arthrotec = diclofenac + misoprostol] Upper GI Drug Regimens For acute ulcer therapy, full dose, and for ulcer prophylaxis, ½ usual dose, given at hs. For example: for active duodenal ulcer, Axid 150 mg bid or 300 mg @ hs. For maintenance therapy, Axid 150 mg @ hs For drug-induced ulcer prophylaxis, Cytotec, 100-200 mcg qid pc and hs or 200 mcg bid or tid - Maximum plasma concentrations are diminished when taken with food. Because of GI side effects of abdominal pain and nausea, manufacturer recommends that drug be taken with food. - Diarrhea is also a common side effect and is dose-related. It is usually selflimiting (often resolving in 8 days). The incidence of diarrhea can be minimized by taking the drug after meals and at bedtime. 5 NOTE: “Symptomatic response to therapy does not preclude the presence of gastric malignancy.” Nausea and Vomiting Basics Vomiting, or emesis, is the forcible emptying or expulsion of gastric and occasionally intestinal contents through the mouth. Signals from 1) the gastrointestinal tract, 2) the labyrinth, and the 3) cortex go to the 4) chemoreceptor trigger zone (CTZ) which then send the message to the 5) vomiting center in the medulla. These signals are sent via neurotransmitters: - Dopamine (GI tract and CTZ) - Histamine 1 (vestibular, vomiting center, and labyrinth pathways) - Prostaglandins (GI tract) - Serotonin (5 HT3) (GI tract, CTZ, and vomiting center) - Acetylcholine (ACh) (vestibular, vomiting center, and labyrinth pathways) The drugs used as antiemetics effect these neurotransmitters: - ACh is blocked by anticholinergic drugs - Histamine 1 is blocked by antihistamines (H1 receptor blockers) - Dopamine is blocked by neuroleptic agents and prokinetic agents - Serotonin is blocked by serotonin blockers (5-HT3 antagonists) The drugs used as antiemetics work on each of these areas: Antiemetics Area Gastrointestinal Tract Labyrinth Cortex Chemoreceptor trigger zone Vomiting center (medulla) Types of Drugs Affecting Area - Prokinetic drugs - Serotonin blockers - Anticholinergics - Antihistamines - Neuroleptics - Prokinetic drugs - THC (tetrahydrocannabinoid) = the major psychoactive substance in marijuana - Neuroleptics - Prokinetic drugs - Serotonin blockers - Serotonin blockers 6 Let’s look at each of the categories of antiemetics: Examples Mechanism of Action Therapeutic Effects Common Drug Interactions Adverse Effects Category: Anticholinergics Scopolamine Block ACh receptors in the vestibular nuclei and reticular formation Motion sickness, secretion reduction before surgery, nausea and vomiting With antihistamines and antidepressants, additive effect increased anticholinergic effects (drying effects) Rash, erythema, difficult urination, dizziness, drowsiness, disorientation, blurred vision, dilated pupils, dry mouth Category: Antihistamine (H1 receptor blockers) Examples Promethazine (Phenergan), meclizine (Antivert), diphenhydramine (Dramamine) Mechanism of Action Block histamine 1 receptors, thereby preventing ACh from binding to receptors in the vestibular nuclei Therapeutic Effects Motion sickness, nonproductive cough, sedation, rhinitis, allergy symptoms, N & V Common Drug Interactions With barbiturates, narcotics, hypnotics, tricyclic antidepressants, alcohol, additive effect increased CNS depression Adverse Effects Dizziness, drowsiness, confusion, urinary retention, blurred vision, dilated pupils, dry mouth 7 Category: Neuroleptic agents Chlorpromazine (Thorazine), prochlorperazine (Compazine) Mechanism of Action Block dopamine in the CTZ and may also block ACh (** Not for use with Parkinson’s) Therapeutic Effects Psychotic disorders (mania, schizophrenia, anxiety), intractable hiccups, N & V Common Drug Interactions Blocks levodopa, which may cancel the beneficial effects of levodopa in treatment of Parkinson’s disease. With quinidine, additive effect increased adverse cardiac effects Adverse Effects Orthostatics hypotension, ECG changes, tachycardia, blurred vision, dry eyes, dry mouth, N & V, anorexia, constipation, urinary retention, extrapyramidal symptoms, pseudoparkinsonism, akathisia, dystonia, tardive dyskinesia, headache Examples Category: Prokinetic Agents Examples Metoclopramide (Reglan), cisapride (Propulsid)** ** Problem with Cytochrome P450 (with Biaxin, emycin, -azoles ventricular arrhythmias) Mechanism of Action Block dopamine in the CTZ or stimulate ACh receptors Therapeutic Effects Increases gastric emptying, GERD, N & V Common Drug Interactions With alcohol, additive effect CNS depression With anticholinergics and analgesics, block antagonism of motility effects of metoclopramide Adverse Effects Sedation, fatigue, restlessness, headache, dystonia, dry mouth, N & V, hypotension, SVT 8 Examples Mechanism of Action Therapeutic Effects Common Drug Interactions Adverse Effects Category: Serotonin blockers Ondansetron (Zofran), granisetron (Kytril) Block serotonin receptors in the GI tract, CTZ, and vomiting center N & V associated with cancer chemotherapy, postop N & V Headache, diarrhea, increased AST and ALT levels, rash, bronchospasm Category: Tetracannabinoids Examples Dronabinol (Marinol) Mechanism of Action Has inhibitory effects on the reticular formation, thalamus, and cerebral cortex Therapeutic Effects N & V associated with cancer chemotherapy Common Drug Interactions Additive effect with other CNS depressants Adverse Effects Drowsiness, dizziness, anxiety, confusion, dry mouth, visual disturbances NOTE: Antiemetics in general should be given before any chemotherapy agent is administered, often 1 to 3 hours beforehand. 9 Problems of Gastrointestinal Motility: Diarrhea and Constipation Diarrhea: - Leading cause of morbidity and mortality in third world countries - 5-8 million deaths per year in infants and children - Loss of time and productivity at work has an enormous financial impact with an estimated cost of $23 billion per year or $108 per person per year in the U.S. - Most acute diarrhea is self-limiting, subsiding in 3 days to 2 weeks - Fluid and electrolyte replacement is vital - Causes of acute diarrhea: o Bacterial o Drug-induced o Viral o Nutritional o Protozoal o Other - Causes of chronic diarrhea: o Tumors o Diabetes mellitus o Hyperthyroidism o Addison’s disease o Irritable bowel syndrome o Other Constipation: Causes - Metabolic and endocrine disorders (DM, hypothyroidism, pregnancy, hypercalcemia, hypokalemia) - Neurogenic disorders (autonomic neuropathy, intestinal pseudo-obstruction, multiple sclerosis, spinal cord lesions, Parkinson’s disease, CVA) - Adverse drug effects (analgesics, anticholinergics, iron supplements, aluminum antacids, calcium antacids, opiates, calcium channel blockers, Vinca alkaloids) - Lifestyle o Poor bowel movement habits (voluntary refusal to defecate resulting in constipation) o Diet (poor fluid intake and/or low-residue (roughage) diets or excessive consumption of dairy products) o Physical inactivity (lack of proper exercise, especially in elderly individuals) o Psychologic (anxiety, stress, hypochondria) 10 Drugs affecting gastrointestinal motility Dealing with Diarrhea Drugs therapy for diarrhea includes: - Adsorbents - Anticholinergics - Opiates - Intestinal flora modifiers Examples Mechanism of Action Adverse Effects Drug Interactions Category: Adsorbents Bismuth subsalicylate (Pepto Bismol), attapulgite (Kaopectate) Coat walls of GI tract, absorbing bacteria or toxins causing diarrhea, and eliminating them with stool With bismuth subsalicylate: increased bleeding time, constipation, dark stools, confusion, twitching, hearing loss, tinnitus, metallic taste, blue gums With digoxin, clindamycin, quinidine: decreased absorption With oral anticoagulants: increased bleeding time, bruising With methotrexate: increased toxicity With probenecid: decreased probenecid effects With hypoglycemia agents: decreased hypoglycemic effects 11 Examples Mechanism of Action Adverse Effects Drug Interactions Examples Mechanism of Action Adverse Effects Drug Interactions Category: Anticholinergics Atropine Decreased intestinal muscle tone and peristalsis, thereby slowing the movement of fecal matter through the GI tract. Often combined with other antidiarrheals to increase their effectiveness Urinary retention and hesitancy, impotence, headache, dizziness, confusion, anxiety, drowsiness, hypotension, HTN, Bradycardia, tachycardia, dry skin, rash, flushing, blurred vision, photophobia, increased pressure in the eye With antacids, decreased anticholinergic effects With amantadine, tricyclic antidepressants, MAOIs, antihistamines increased anticholinergic effects Category: Opiates Opium tincture, paregoric, codeine diphenoxylate (Lomotil), loperamide (Imodium) Cause constipation by lowering the motility of the bowel and relieving rectal spasms. By slowing the time it takes to pass food through the intestines, water and electrolytes have a greater chance of being absorbed, with reduces tool frequency and volume Drowsiness, sedation, dizziness, lethargy, N & V, anorexia, constipation, respiratory depression, bradycardia, palpitations, hypotension, urinary retention, flushing, rash, urticaria Increased CNS depressant effects with CNS depressants, alcohol, narcotics, sedative hypnotics, antipsychotics, skeletal muscle relaxants 12 Examples Mechanism of Action Adverse Effects Drug Interactions Category: Intestinal Flora Modifiers Lactobacillus acidophilus Suppress the growth of diarrhea-causing bacteria and help reestablish the normal intestinal flora that has been depleted by the diarrhea N/A N/A NOTE: alosetron HCl tablets (Lotronex) – was used for irritable bowel syndrome, diarrhea-dominant Withdrawn from US Market in 2000 due to deaths from bowel obstruction Dealing with Constipation: Laxatives and Stool Softeners Drugs for constipation include 5 types: - Bulk-forming - Emollient - Hyperosmotic - Saline - Stimulant/Irritant Examples Mechanism of Action Therapeutic Effects Adverse Effects Drug Interactions Category: Bulk-forming Psyllium, methylcellulose (Metamucil) Absorbs water to increase bulk, distending bowel to initiate reflex bowel activity (onset of action 12 hours to 3 days) Acute constipation, IBS, diverticulosis Impaction above strictures, fluid overload Increased absorption of antibiotics, digoxin, nitrofurantoin, salicylates, tetracyclines, oral anticoagulants Note: Bulk-forming agents: Drug of Choice Note: Psyllium contains sugar: give cautiously in DM 13 Examples Mechanism of Action Therapeutic Effects Adverse Effects Drug Interactions Category: Emollient/Surfactants Docusate salts (Surfak, Colace), mineral oil Wetting agent used to soften fecal mass (onset of action 1-3 days) Acute constipation, softens fecal impacts, facilitates bowel movements in anorectal conditions Skin rashes, decreased absorption of vitamins, lipid pneumonia With mineral oil, increased effect of oral anticoagulants, decreased absorption of fatsoluble vitamins (A, D, E, K) Note: Lipid pneumonia – especially in elderly (inhale the mineral oil) Leakage of oil can cause pruritis ani; disturbs normal defecation reflex Examples Mechanism of Action Therapeutic Effects Adverse Effects Drug Interactions Category: Hyperosmotic Lactulose, sorbitol, glycerine Osmotic molecules (like excess sugar) pulls water into GI tract (onset of action 24-48 hours) Chronic constipation, diagnostic and surgical preparations Caution with diabetics, galactose or lactose intolerance Abdominal bloating, rectal irritation With oral antibiotics, decreased effects of lactulose 14 Examples Mechanism of Action Therapeutic Effects Adverse Effects Drug Interactions Category: Saline Magnesium sulfate, magnesium phosphate, magnesium citrate, MOM Increases water content of feces, resulting in distention, peristalsis, and evacuation (onset of action 1-3 hours) Constipation, removal of anthelmintics and parasites, diagnostic and surgical preparations Magnesium toxicity (with renal insufficiency) With barbiturates, general anesthetics, narcotics, and antipsychotics increased CNS depression With neuromuscular blockers, increased effects Caution: MOM contains high concentration of sodium Watch renal disease! Examples Mechanism of Action Therapeutic Effects Adverse Effects Drug Interactions Category: Simulant/Irritant Castor oil, bisacodyl (Dulcolax) Direct action on intestinal mucosa (onset of action 6-10 hours) Acute constipation, diagnostic and surgical bowel preparations Nutrient malabsorption, skin rashes, gastric irritation, rectal stimulation With antacids and H2 blockers gastric irritation With antibiotics, digoxin, nitrofurantoin, salicylates, tetracyclines, oral anticoagulants decreased absorption Stimulant/Irritant Laxatives: Most commonly abused by teens and elderly NOTE: Long-term use may lead to laxative dependence. 15 Zelnorm (tegaserod maleate): New medication (2004) for constipation-dominant IBS A serotonin 5-HT4 receptor partial agonist For short-term treatment of women who have IBS with constipation as their main bowel problem FDA warning in May 2004: Zelnorm associated with serious consequences of diarrhea and ischemic colitis Withdrawn from market in 2007 due to risks of serious CV events Amitiza (lubiprostone) For treatment of chronic idiopathic constipation in adults Locally acting chloride channel activator that enhances a chloride-rich intestinal fluid secretion without altering sodium and potassium concentrations in the serum Contraindicated in patients with a history of mechanical GI obstruction, severe diarrhea Adverse effects: nausea, diarrhea….Take with food to decrease nausea Dose: 24 mcg twice daily orally with food Linzess (linaclotide) For treatment of both irritable bowel syndrome with constipation and chronic idiopathic constipation Is a guanylate cyclase-C (GC-C) agonist; acts locally on the luminal surface of the intestinal epithelium to increase cyclic guanosine monophosphate (cGMP) which stimulates secretion of chloride and bicarbonate into the intestinal lumen. Adverse effects: diarrhea, abdominal pain Dose: 290 mcg capsule taken once daily on an empty stomach at least 30 minutes before the first meal of the day. Drugs for chronic inflammatory bowel: Ulcerative colitis o Sulfasalazene 2 Gm (Azulfidine) o Steroids helpful during symptom flare, but not useful for prevention of flare Crohn’s o Azothioprine (Imuran), Cromolyn