Quality Improvement Organizations
advertisement

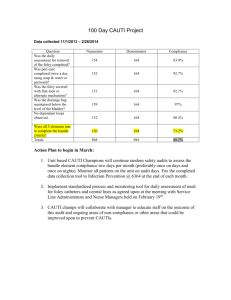
10th SOW Wrap-Up Karline Roberts & William Gardiner July 24, 2014 Overview • • • • • • • • • Project began August 1, 2011 58 hospitals participated 4 face to face LAN meetings 24 webinars CUSP Training CAUTI workgroup call series Handwashing for Life visits ATP monitoring Countless site visits 2 Tools •HAI Resource Guide •RCA Tool Kit •CLABSI Video •CLABSI Maintenance Bundle •Excel Audit tool for CLABSI & CAUTI •CLIP monitoring form •Hand washing pins •PowerPoint templates for CLABSI, CAUTI, CDI 3 More Tools •CAUTI Posters – 3 •CAUTI Screen Savers •Foley Insertion Checklist •CAUTI Patient Brochure •CAUTI Pocket Card •Patient Hand washing Brochure •CDI Bundle •CDI Tool Kit •SSI Pocket card •Antibiotic Selection Pocket cards 4 IPRO website http://qio.ipro.org/hospitals-hai/about-thisproject/prevention-tools-and-resources-for-healthcareprofessionals 5 Advisory Committee Members •Brian Koll, MD – Mt. Sinai Beth Israel Medical Center •Zeynep Sumer - GNYHA •Ghinwa Dumyati, MD - University of Rochester •Mary Ann Magerl - Vassar Brothers •Kathi Mullaney - Metropolitan Hospital •Christina Ostwald - Mount St. •Hillary Jalon - United Hospital Fund •Mary Manfredo – Oneida Hospital •Mary Therriault - HANYS •Carol VanAntwerpen •David Calfee, MD - New York Presbyterian/Weil Cornell Center •Peggy A. Hazamy –DOH •Donna Armellino - North Shore Hospital System Mary's •Mary Jane Milano - Regional Hospital Association 6 CLABSI Relative Improvement 7 CLABSI SIR 8 CLIP Adherence was consistently well over 90% No CLIP for 11th SOW!!! 9 CAUTI Relative Improvement 10 CAUTI SIR 11 Standardized Urinary Catheter Utilization Rate (SDUR) 12 CDI Relative Improvement 13 CDI SIR 14 10th SOW Overview - Barriers and Successful Interventions Antimicrobial Stewardship Barriers: a. Lack of administrative support b. Lack of an ID physician c. Lack of a clinical pharmacist d. Overwhelmed ID physician e. Lack of running and/or distribution of an (annual) antibiogram f. Lack of formulary restrictions g. Lack of agreement in what constitutes an acceptable program h. Not knowing where to start i. Lack of budgetary resources Successful Interventions: a. Starting with one intervention with gradual expansion, once support is demonstrated b. The lab culture not only contains the susceptibility results but also contains the price of the antibiotics, so practitioners can equate the cost of therapy. c. Selected antibiotics require an ID consult d. Antibiograms are run (annually, biannually) and distributed to practitioners via pocket cards e. Antibiogram is on the back of the antibiotic order sheet. Catheter Related Urinary Tract Infections (CAUTI) Barriers: a. Lack of administrative support or a physician champion b. Lack of demonstrated competency for insertion and maintenance of foley catheters c. Receipt of patients with foley catheters already in place d. Lack of a daily reminder system to remove the foley. e. Lack of appropriate reasons for foley insertion a. Lack of clinician understanding of what is considered “appropriate” f. Lack of delivery of the urine specimen to the laboratory in a timely manner or proper refrigeration g. Manual daily foley counts h. Inability to capture foley counts in the EMR i. Foleys are addressed on rounds, but an ordering practitioner does not participate. This hinders an order being written and carried out. j. Lack of a root cause analysis for each infection. k. Lack of a nurse-driven protocol and need for a cultural change for acceptance of the nurse driven protocol. (reluctance to remove a catheter without an ‘order’) l. Lack of a renewal timeframe m. Lack of a good female alternative n. Noncompliant patients disrupting device o. Lack of clinical and surveillance definition consensus. p. Increasing frequency of yeast (mainly Candida spp.), which may not be a true infection q. Lack of IP presence on product evaluation committees and purchasing committees 15 What’s Next? • • • • • • 11th SOW begins August 1st Introductory webinar will be held on August 6th Conditions are: CLABSI, CAUTI, CDI, VAE 5 Year Project Work to be done in ICU and non-ICU units QIOs required to report to CMS the hospitals that continue work from 10th to 11th SOW • New MOA will need to be signed • Work will be done in a community collaborative setting 16 Questions 17 This material was prepared by IPRO, the Medicare Quality Improvement Organization for New York State, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services. The contents do not necessarily reflect CMS policy. 10SOW_NY_AIM7.1-14-08 For more information Karline Roberts Director (518) 320-3508 Karline.roberts@hcqis.org William Gardiner Senior QI Specialist (518) 320-3505 William.gardiner@hcqis.org IPRO CORPORATE HEADQUARTERS 1979 Marcus Avenue Lake Success, NY 11042-1002 IPRO REGIONAL OFFICE 20 Corporate Woods Boulevard Albany, NY 12211-2370 www.ipro.org Template 1/13/2012