template_for_cautixs_05082012
advertisement
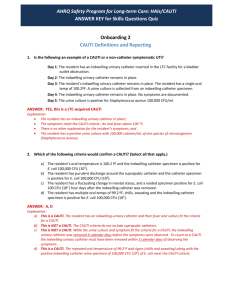
Healthcare Associated Infections (HAI Project) CAUTI’s (Insert your hospital name) In Partnership with IPRO Date CMS Leads a national healthcare quality improvement program, implemented locally by an independent network of QIOs in each state and territory. IPRO The federally funded Medicare Quality Improvement Organization (QIO) for New York State, under contract with the Centers for Medicare & Medicaid Services (CMS). IPRO provides a full spectrum of healthcare assessment and improvement services that foster the efficient use of resources and enhance healthcare quality to achieve better patient outcomes. 2 The QIO Program Largest federal program dedicated to improving health quality at the local level, Trustworthy partners for the continual improvement of healthcare for all Americans, Focuses on three broad aims: Better patient care, Better population health, Lower healthcare costs through improvement. 3 As the QIO for New York State, IPRO works to achieve the goals of the national QIO Program by: • Convening communities of providers, practitioners, and patients across the state to: • Share knowledge • Spread best practice • Achieve rapid, wide-scale improvements in patient care 4 Improving Individual Patient Care Reducing Healthcare-Associated Infections (HAI’s) HAI-Overview APIC Statement on the Cost of Hospital-Associated Infections1 • 2 million patients per year • ~90,000 deaths • $4.5-$5.7 billion per year in patient care costs HAI - Overview HAIs rank in the top 10 leading causes of death in the US2 7 From the Organization’s Perspective HAIs harm the bottom line • Hospital-acquired conditions lead to loss of revenue. 8 National Healthcare Safety Network NHSN Data Collection • The NHSN will become the national repository of data • The infection prevention department is usually responsible for reporting data into NHSN • Data will be available on a facility, state, and national level 9 Improving Individual Patient Care Catheter Associated Urinary Tract Infections CAUTI’s CAUTI – Background An estimated 1 in 4 hospitalized patients received an indwelling urinary catheter in 20034 • ~50% of these indwelling urinary catheters are unnecessary5 • CMS designates CAUTI as a “never event” • Medicare Modernization Act of 2003 • Deficit Reduction Act of 2005 • As of Oct. 1, 2008, no CMS reimbursement • 2007 study showed 12,185 CAUTIs costing $44,043/hospital stay6 • 2012 National Patient Safety Goal • Focuses on CAUTI evidence based prevention for indwelling catheters in hospital and critical access hospital accreditation programs 11 CAUTI – Background CAUTI Characteristics: • Most common site of HAI. • Almost all are caused by instrumentation CAUTI Complications: • Discomfort • Prolonged hospital stay • Increased cost 12 CAUTI Goals Measure Project Target CAUTI Relative Improvement Rate ≥25% Reduction Urinary Catheter Utilization Rate Relative improvement of 10% or greater 13 Sources for CAUTI Guidelines Sources for CAUTI Guidelines APIC - Association for Professionals in Infection Control and Epidemiology http://www.apic.org/Resource_/EliminationGuideForm/c0790db8-2aca4179-a7ae-676c27592de2/File/APIC-CAUTI-Guide.pdf HICPAC - Healthcare Infection Control Practices Advisory Committee http://www.cdc.gov/hicpac/cauti/001_cauti.html SHEA - Society for Healthcare Epidemiology of America http://www.jstor.org/stable/pdfplus/10.1086/591066.pdf?acceptTC=true 15 APIC Guideline Examples • Use indwelling catheters only when medically necessary • Allow only trained healthcare providers to insert catheters • Maintain a sterile closed drainage system • Properly secure catheters after insertion to prevent movement and urethral traction • Maintain drainage bag below level of bladder at all times • Remove catheters when no longer needed • Document indication for urinary catheter on each day of use • Use reminder systems to target opportunities to remove catheters 16 HICPAC Guideline Examples 17 SHEA Guideline Examples • Ensure that trained personnel insert catheters • Practice hand hygiene • Evaluate necessity of catheterization • Review ongoing need regularly • Use smallest gauge catheter possible • Use barrier precautions for insertion • Perform antiseptic cleaning of meatus • Maintain a sterile, closed draining system • Replace system if a break in asepsis occurs • Empty the collecting bag regularly, using a separate collecting container for each patient, and avoid allowing the draining spigot to touch the collecting container 18 References 1. APIC Cost of Hospital-Associated Infections Model. 2. 3. 4. 5. 6. http://www.apic.org/Content/NavigationMenu/PracticeGuidance/Guidelines Standards/APICCostCalculator-Lit051011.xls Klevens RM, Edwards JR, Richards CL, et al. Estimating healthcareassociated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007; 122:160-167. http://www.cdc.gov/ncidod/dhqp/pdf/hicpac/infections_deaths.pdf Perenchvich EN, et al. Raising Standards While Watching the Bottom Line: Making a Business Case for Infection Control. Infect Control Hosp EPID 2007; 28:1121-1133 Smith JM. Indwelling catheter management: from habit-based to evidencebased practice. Ostomy Wound Manage 2003;49:34-45. Gokula RM, Hickner JA, Smith MA. Inappropriate use of urinary catheters in elderly patients at a midwestern community teaching hospital. Am J Infect Control 2004;32:196-199. Wald HL, Kramer AM. Nonpayment for Harms Resulting From Medical Care. JAMA 2007;298: 2782-2784. What we do here (hospital name) Our current urinary catheter policy is: Outline your policy and clearly state what is expected. • Who can insert a urinary catheter? • Is a check list followed? Is you existing policy in agreement with published guidelines • Review current guidelines and compare them to your current policy. Consider updating, as appropriate 21 Our current urinary catheter procedure is as follows: Outline your procedure and discuss any areas you have identified that are in and out of compliance • Does your policy address catheter removal? Do you verbally ask the attending physician if the catheter can be removed on a daily basis? • Is training a component of your procedure? 22 Our current results are as follows: Outline your results and provide any graphs and data to demonstrate where you were when you began your CAUTI project and where you are now. Use run charts to display data over time. Include any interventions which have contributed to improving care and/or modifying procedures. 23 Our Procedure is as follows: After discussing your policy and procedure, ask you staff the following two questions: •Please describe how you think the next patient with a urinary catheter will be harmed. •What can be done to prevent/minimize harm? 24 Our Improvement Plan is as follows: Outline the next steps for your organization to improve or “hold the gains”. Has this project been spread to the entire organization? If not, do you have a target data to move the project house-wide? If no, consider setting a date 25 This material was prepared by IPRO, the Medicare Quality Improvement Organization for New York State, under contract with the Centers for Medicare & Medicaid Services (CMS), an agency of the U.S. Department of Health and Human Services. The contents do not necessarily reflect CMS policy. 10SOW-NY-AIM7.1-12-10 26 Contacts for the HAI Project IPRO Contacts Karline Roberts (518) 320-3508 kroberts@nyqio.sdps.org Bill Gardiner (518) 320-3505 wgardiner@nyqio.sdps.org Crystal Isaacs (516) 209-5589 cisaacs@nyqio.sdps.org Chad Wagoner (518) 320-3552 cwagoner@nyqio.sdps.org Teré Dickson, MD tdickson@nyqio.sdps.org (516) 209-5324 Hospital Contacts Fill in the names of your hospital contacts