CUSP/CAUTI Content Call #2
advertisement

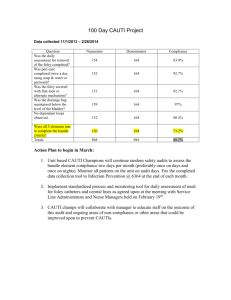
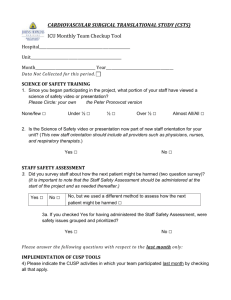
On the CUSP: Stop CAUTI The Science of Improving Patient Safety Sean Berenholtz, MD MHS Johns Hopkins University Quality and Safety Research Group 1 CAUTI Content Call Schedule CUSP/CAUTI Content Call #1 – CUSP Moderator – Sam Watson; Speaker – Sean Berenholtz 03/07/11 2 ET/1 CT/12 MT/11 PT Attendee: (866) 256-9295 CUSP/CAUTI Content Call #2 - The Science of Safety Moderator – Sam Watson; Speaker – Sean Berenholtz 03/22/11 2 ET/1 CT/12 MT/11 PT Attendee: (866) 256-9295 CUSP/CAUTI Content Call #3 - Care and Removal Intervention Moderator – Sam Watson; Speaker – Mohamad Fakih 04/05/11 2 ET/1 CT/12 MT/11 PT Attendee: (866) 256-9295 CUSP/CAUTI Content Call #4 - Data Collection Moderator – Sam Watson; Speaker – Christine George 04/19/11 2 ET/1 CT/12 MT/11 PT Attendee: (866) 256-9295 CUSP/CAUTI Content Call #5 - The View from the Bedside Moderator – Sam Watson; Speaker – Russ Olmsted 05/03/11 2 ET/1 CT/12 MT/11 PT Attendee: (866) 256-9295 CUSP/CAUTI Content Call #6 - Implementation in a Community Hospital Moderator – Sam Watson; Speaker – Mary Jo Skiba 05/17/11 2 ET/1 CT/12 MT/11 PT Attendee: (866) 256-9295 2 60 Min. 60 Min. 60 Min. 60 Min. 60 Min. 60 Min. The Marvel of Modern Medicine 3 4 The Problem is Large • In U.S. Healthcare system – 7% of patients suffer a medication error 2 – On average, every patient admitted to an ICU suffers an adverse event 3,4 – 44,000- 98,000 people die each year as the result of medical errors 5 – Nearly 100,000 deaths from HAIs 6 – Estimated 30,000 to 62,000 deaths from CLABSIs 7 – Cost of HAIs is $28-33 billion 7 • 8 countries report similar findings to the U.S. Bates DW, Cullen DJ, Laird N, et al., JAMA, 1995 Donchin Y, Gopher D, Olin M, et al., Crit Care Med, 1995. Andrews L, Stocking C, Krizek T, et al., Lancet, 1997. Kohn L, Corrigan J, Donaldson M., To Err Is Human, 1999. Klevens M, Edwards J, Richards C, et al., PHR, 2007 Ending Health Care-Associated Infections, AHRQ, 2009. 5 Healthcare-Associated Infections: A Preventable Epidemic • Focus on 4 HAIs: VAP, SSI, CRBSI, UTI • $5 billion per year excess costs • 1.7 million patients per year – 1 out of 20 patients • 98,000 deaths per year – As many deaths as breast cancer and HIV/AIDS put together – 6th leading cause of preventable deaths http://oversight.house.gov/story.asp?id=1865 6 7 How Can These Errors Happen? • People are fallible • Medicine is still treated as an art, not science • Need to view the delivery of healthcare as a science • Need systems that catch mistakes before they reach the patient Caregivers are not to blame 8 On the CUSP: Stop CAUTI Rather than being the main instigators of an accident, operators tend to be the inheritors of system defects….. Their part is that of adding the final garnish to a lethal brew that has been long in the cooking.” James Reason, Human Error, 1990 9 System Factors Impact Safety Institutional Hospital Departmental Factors Work Environment Team Factors Individual Provider Task Factors Patient Characteristics Adapted from Vincent 10 Case Example • • • • • • 65 yo M s/p lung resection for cancer Admit to ICU; discharged to floor POD 1 POD 3 develops hypoxia Admitted to ICU, intubated CXR shows extensive left lung collapse Decision to perform broncoscopy 11 11 System Failure Leading to Error Did not verify equipment availability Fatigue Bronch cart not stocked Patient suffers Communication between resident and nurse Hypoxic arrest 12 Principles of Safe Design • Standardize – Eliminate steps if possible • Create independent checks • Learn when things go wrong – – – – What happened Why What did you do to reduce risk How do you know it worked 13 Eliminate Steps 14 Create Independent Checks 15 Design Examples Standardization Redundancy 16 EVIDENCE-BASED BEHAVIORS TO PREVENT CLABSI • Remove Unnecessary Lines • Wash Hands Prior to Procedure • Use Maximal Barrier Precautions • Clean Skin with Chlorhexidine • Avoid Femoral Lines MMWR. 2002;51:RR-10 17 Standardize 18 CR-BSI Checklist • Before the procedure, did they: – Wash hands – Sterilize procedure site – Drape entire patient in a sterile fashion • During the procedure, did they: – Use sterile gloves, mask and sterile gown – Maintain a sterile field • Did all personnel assisting with procedure follow the above precautions • Empowered nursing to stop the procedure if violation occurred Crit Care Med 2004;32(10):2014. 19 Michigan Keystone ICU 9 8 7 6 5 4 3 2 1 0 B In as te el rv in e e n ti o n 0 -3 4 -6 7 1 9 0 -1 1 2 3 -1 1 5 6 -1 1 8 9 -2 2 1 2 -2 2 4 5 -2 2 7 8 -3 3 0 1 -3 3 3 4 -3 6 CRBSI Rate Me dia n a nd Me a n CRBSI Ra te Time (mont hs) M e d ia n C R B S I R a te M e a n C R B S I R ate NEJM 2006, BMJ 2010 20 Rhode Island ICU CLABSI Rates Qual Saf Health Care 2010;19(6):555-561 21 Improving Care for Ventilated Patients • Semirecumbant positioning • Peptic ulcer disease and DVT prophylaxis • Appropriate sedation • Daily assessment of readiness to extubate • Oral care with antiseptics 22 Improving Care for Ventilated Patients • Educate staff • Decrease complexity / create redundancy: – Standardized order sets and protocols – Daily goals checklist • Other independent redundancies – Nursing and families – Are patients receiving the prevention they should? 23 Daily Goals • What needs to be done for the patient to be discharged? • What is the patients greatest safety risk? • What can we do to reduce the risk? • Can any tubes, lines, or drains be removed? J Crit Care 2003;18(2):71-75 24 Michigan Keystone ICU Infect Control Hosp Epidemiol. 2011 25 Preventing Catheter-Associated Urinary Tract Infection • Most common healthcare-associated infection (~ 40%) • Many urinary catheters used inappropriately 1 • Prevention guidelines: – HICPAC www.cdc.gov/hicpac/pdf/CAUTI/CAUTIguideline2009final.pdf – SHEA/IDSA: Infect Control Hosp Epid 2008;29:S41-S50 • Nurse-Led multidisciplinary rounds to reduce unnecessary urinary catheters 2 • Urinary catheter reminders and stop-orders decrease infection rates 3 1 Saint S, et al. Am J Med 2000 2 Fakih MG, et al. Infec Control Hosp Epi 2008 3 Meddings J et al. Clin Infect Dis 2010 26 On the CUSP: Stop CAUTI Principles of Safe Design Apply to Technical and Team Work 27 Basic Components and Process of Communication Dayton E, Henriksen K, Jt Comm J Qual Patient Saf, 2007. 28 28 Teamwork Tools • Daily Goals • AM briefing • Shadowing • Culture check up • TeamSTEPPS 29 Teams Make Wise Decisions When There is Diverse and Independent Input • Wisdom of Crowds • Alternate between convergent and divergent thinking • Get from the dance floor to the balcony level Heifetz R, Leadership Without Easy Answers,1994. 30 Summary • Develop lenses to see systems • Understand principles of safe design – standardize, – create redundancies, – learn when things go wrong • Recognize these principles apply to technical and team work • Teams make wise decisions when there is diverse and independent input 31 Action Items • Have all members of the CUSP CAUTI Team view the Science of Improving Patient Safety video • Put together a roster of who on your unit needs to view the Science of Safety video • Develop a plan to have all staff on your unit view the Science of Improving Patient Safety video – Assess what technologies you have available for staff to view – Identify times for viewing it (e.g., staff meetings, individual admin hours) 32 33