Presentation
advertisement

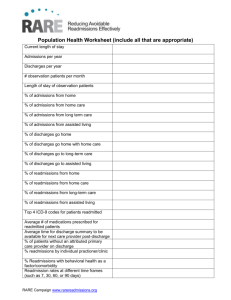
Improving Harm Across the Board Kathleen M. Louth Director of Quality Management Monroe County Hospital P. O. Box 1068 Forsyth, GA 31029 478.994.2521 ext. 2150 klouth@monroehospital.org Hospital Trend Rate in Reducing Harm Harms/1,000 discharges 30% 25% 20% 15% 10% 5% 0% Q1 11 Q2 11 Q3 11 Q4 11 Q1 12 Q2 12 Q3 12 Q4 12 Q1 13 *HAC harm = inpatient hospital acquired conditions 2 Number of Harms 10 9 8 7 6 5 4 3 2 1 0 Q1 11 Q2 11 Q3 11 Q4 11 Q1 12 Q2 12 Q3 12 Q4 12 Q1 13 3 30 Day Total Readmission Rate All Cause 30% 27.91% 25% 21.28% 20% 15% 18.00% 16.36% 13.16% 12.96% 11.11% 10% 9.09% 9.52% 5% 0% Q1 11 Q2 11 Q3 11 Q4 11 Q1 12 Q2 12 Q3 12 Q4 12 Q1 13 *all cause 30 day readmissions 4 Number of Readmissions All Cause 14 12 12 10 10 9 9 8 7 6 6 5 4 4 4 2 0 Q1 11 Q2 11 Q3 11 Q4 11 Q1 12 Q2 12 Q3 12 Q4 12 Q1 13 5 Pearls Multidisciplinary •It is not just the work of the Quality Improvement Department; all departments must be involved • Must be a collaborative effort from the top-down and bottom-up • Increased communication and input from management staff Assign ownership and expectations • Establish timelines for project deliverables •Continue to meet with definite reporting timeframes Educate •Keep the staff, medical staff, and board informed Defining Moments In Our Journey Defining Moments & Commitment to Patient Safety: • 2009-New CEO who had experience in Quality & Patient Safety; new Director of Quality Management hired • 2010- Patient Safety Plan & Commitment to Patient Safety developed; revised incident reporting system & tools; fall team formed; medication error team formed; Quality Council & reporting revised; education of changes to all (hospital wide); Culture of Patient Safety Survey implemented; Patient Safety Week recognized •2011-Fall prevention program revised; education of changes to all (hospital wide); Glycemic Control team formed; CLABSI team formed 7 Defining Moments In Our Journey • 2012- Participation in the Hospital Engagement Network (HEN) & education to management team; Regrouped on readmissions due to data issues; formation of Readmission Reduction team; OATS team formed; HCAHPS training; CAUTI team formed; Marketing of Patient Safety through website, banners, boards, & local newspaper • 2013-Strategies to reduce readmissions implemented-bedside shift reporting, white boards, rounding (hourly, nurse manager, leadership), discharge follow up calls, follow up appointments made, discharge folder, pharmacist educating high risk patients, follow up calls for ER patients, working with hospice and home heath agencies, participating in GMCF Care Transitions, participating in MATCH, Patient & Family Engagement; Case Manager position job duties aligned with reducing readmission efforts to include discharge process Breakthrough Strategy • Major Challenges Encountered – – – – Limited Resources (human, time, financial) Implementation of EHR Culture change Training • Strategies to Overcome – – – – Time management, utilizing resources from the HEN Constant education and re- education, dedicated point person for EHR Reinforcement of rationales, hearing stories from peers at other facilities Make it fun, pertinent, convenient, personal, and using personalized teaching methods Risk Profile: The Areas of Risk We Are Committed To Controlling Annual discharges: 378 year 2010 Slide 10 HAC risk opportunities/discharge: 4.37 HACs Estimated annual number of patients at risk in each area Number of Opportunities ADE # of discharges: 378 CAUTI # pts in IP units with catheter in place: 127 CLABSI # pts in IP units with central lines: 0 Falls # of discharges: 378 Ob AE # of women with deliveries: 0 Pr Ulcer # of discharges: 378 SSI # of inpatient surgeries: 15 VAP # of patients on a ventilator: 0 VTE # of discharges: 378 EED # of women with elective deliveries 0 TOTAL Risk opportunities for harm across the board 1654 Readmit # of inpatients at risk of readmit: 378 Slide 11 Our improvement journey Improvement Scale: The stages we move through Number of risk areas (0-11) at each stage IDEAL: level represents zero harm 7 At Target: level represents meeting improvement target 1 Progress: level shows movement but not yet at target 0 Opportunity: level is an opportunity to launch aggressive action 0 Improving Harm Rates (per discharge) HACs Baseline Rate [2010] Target Rate ADE 0% 0% CAUTI 0% 0% CLABSI 0% 0% Falls 0% 0% Ob AE 0% 0% Pr Ulcer 0% 0% SSI 0% 0% VAP 0% 0% VTE 0% 0% EED 0% 0% Total 0% 0% Readmit 15.15% 15.24% Improving Harm Rates (per discharge) HACs Baseline Rate [2010] Target Rate Current Rate [2012] Improvement Status (scale) ADE 0% 0% 0% IDEAL CAUTI 0% 0% 0% IDEAL CLABSI 0% 0% 0% IDEAL Falls 0% 0% 0% IDEAL Ob AE 0% 0% 0% N/A Pr Ulcer 0% 0% 0% IDEAL SSI 0% 0% 0% IDEAL VAP 0% 0% 0% N/A VTE 0% 0% 0% IDEAL EED 0% 0% 0% N/A Total 0% 0% 0% IDEAL Readmit 15.15% 15.24% 14.47% Target Our Hospital Risk Score Card Our Safety Mandate Annual Volume (Discharges) 378 Total risk: annual harm opportunities 1654 Risks per patients (Total Opportunities)/Discharges) 4.37 Number of Risk Areas Number of PfP Risk Areas Applicable (0 – 11) 8 Number of PfP Risk Areas Applicable & Adopted 8 Our Progress Number of PfP Areas with Major Improvement Opportunity 0 Number of PfP Areas at Improvement Target 1 Number of PfP Areas at IDEAL 7 Pictured 1st row left to right: Shawnelle Lupton, Operating Room Nurse Manager; Dr. Dana Peterman, PT, DPT; Casey Fleckenstein, Medical/Surgical Nurse Manager Pictured 2nd row left to right: Dr. Craig Caldwell, Past President of the Medical Staff/Hospital Authority Board Member; Sherry Mays, Clinical Coordinator; Kathleen Louth, Director of Quality Management; and Tim Allen, Director of Engineering and Environmental Services. Not pictured: Kay Floyd, CEO; Tony Ussery, Chairman of the Quality Council/Vice Chairman of the Hospital Authority Board; Megan Randall, Director of Radiology; Pam Lankford, Emergency Room Nurse Manager; Hugh Cromer, Director of Pharmacy; Laura Roush, Director of Laboratory; Jean Riley, Director of Respiratory Therapy/Infection Control; Cindy Renno, Dietary Manager; Ticia Hicks, Case Management; Michelle Wiggins, Swing Bed Coordinator; and Mamie Patterson, Diabetes Support Group. Next big step to Reduce Harm • Continue our efforts that we already started • Enhance patient & family engagement • Implement teach back