Hyperemesis Gravidarum - Philadelphia University
advertisement

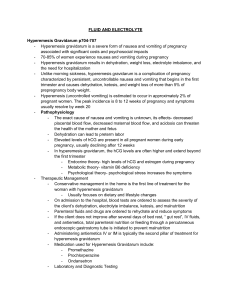
Hyperemesis Gravidarum Learning objective Identify Hyperemesis Gravidarum • Differentiate between morning sickness • and Hyperemesis Gravidarum Describe the complications of • Hyperemesis Gravidarum Explain management of Hyperemesis • Gravidarum Discus nursing role of Hyperemesis • Gravidarum • Outline : * Introduction Hyperemesis Gravidarum * Introduction Pathophysiology Clinical Manifestations Complications Diagnostic Evaluation Management Introduction Hyperemesis Gravidarum At lest 80% of women experience nausea &vomiting. The term morning sickness is often used to describe this condition when symptoms usually disappear after the first trimester. this mild form affects he quality of life of women &her family where the sever form hyperemesis gravidarum results in dehydration ,electrolyte imbalance and the need for hospitalization Identification Unlike morning sickness, hyperemesis gravidarum: is a complication of pregnancy characterized by persistent uncontrollable nausea and vomiting that persists beyond the 20th week of pregnancy . Pathophysiology Causes : numerous theories abound, but few studies have produced scientific evidence to identify the etiology of this condition it is likely that multiple factors contribute to it . Pathophysiology Elevated Level OF HCG are present in all pregnant women during early pregnancy, usually declining after 12 week .this corresponds to the usual duration of morning sickness .in hyperemesis gravidarum ,the Pathophysiology decrease fluid intake& prolonged vomiting cause dehydration which increase serum concentration of hCG ; Pathophysiology Endocrine theory :high levels of hCG & estrogen during pregnancy Metabolic theory :vitamin B6 deficiency Psychological theory : Psychological stress increase the symptoms Complication Weight loss Dehydration Metabolic acidosis from starvation Alkalosis from loss of HCL Hypokalemia (electrolyte imbalance) Nursing Role Nursing Assessment Health history &physical • examination: asking the client about the onset, duration ,and course of her nausea and vomiting Ask her about any medication or treatments she used and how effective they were in relieving her nausea and vomiting obtain a diet history from the client including a dietary recall for the past week Nursing Assessment Note the client’s knowledge of nutrition &need for appropriate nutritional intake Also ask about any complaints of ptyalism . Ask if she has any noticed any blood or mucus in her stool Weight the client. Nursing Assessment Inspect the mucous membranes for dryness &check skin turgor for. Assess blood pressure for changes . Note any complaints of weakness ,fatigue, activity intolerance ,dizziness, or sleep disturbance Laboratory & Diagnostic test Liver enzyme: elevation of (AST) & (ALT) are usually present. CBC: elevated level of RBC & hematocrite indicating dehydration. Urine ketones: positive when the body breaks down fat to provide energy in the absence IIT Laboratory & diagnostic test BUN :increase in the presence of salt &water depletion Urine specific gravity :grater than 1.025indicating concentrated urine linked to inadequate fluid intake Serum electrolyte decrease levels of k, Na, Cl Ultrasound :evaluation for molar or multi pregnancy Diagnosis Fluid & electrolyte imbalance Impaired nutrition intake Knowledge deficit Intervention Maintain NPO status to allow GI tract to rest Administer antiemetic drugs like : promethazine,prchlorperazine,odanse -tron. Administer IV fluid like 5% dextrose in lactated ringer Administer electrolyte replacement therapy Hygiene measures and oral care Pay special attention to the environment making sure to keep the area free of pungent odors As the Client's nausea and vomiting subside .gradually introduce oral fluid &foods in small amounts Monitor intake and output Offer reassurance that all intervention are directed toward promoting positive pregnancy outcomes for both women fetus Provide information about the expected plan of care Listen to here concerns &feeling by answering all here questions Teach the client about therapeutic life style changes like avoid stressors& fatigue Avoid noxious stimuli Avoid tight waistband Eat small frequent meals (6 meals) Separate fluid from solid by consuming fluid In between meals Use high protein supplement Avoid lying down for at least 2 hours after eating Avoid food high in fat drink herbal tea eat food that settle the stomach such as toast or soda References From this book Susan scote ricci & terri Kyle.(2009) • Maternity and pediatric nursing ,chapter19, pregnancy related complication , page 567-569