
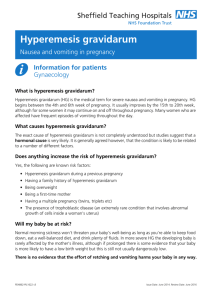
FLUID AND ELECTROLYTE Hyperemesis Gravidarum p704-707 - Hyperemesis gravidarum is a severe form of nausea and vomiting of pregnancy associated with significant costs and psychosocial impacts - 70-85% of women experience nausea and vomiting during pregnancy - Hyperemesis gravidarum results in dehydration, weight loss, electrolyte imbalance, and the need for hospitalization - Unlike morning sickness, hyperemesis gravidarum is a complication of pregnancy characterized by persistent, uncontrollable nausea and vomiting that begins in the first trimester and causes dehydration, ketosis, and weight loss of more than 5% of prepregnancy body weight. - Hyperemesis (uncontrolled vomiting) is estimated to occur in approximately 2% of pregnant women. The peak incidence is 8 to 12 weeks of pregnancy and symptoms usually resolve by week 20 - Pathophysiology - The exact cause of nausea and vomiting is unknown, its effects- decreased placental blood flow, decreased maternal blood flow, and acidosis can threaten the health of the mother and fetus - Dehydration can lead to preterm labor - Elevated levels of hCG are present in all pregnant women during early pregnancy, usually declining after 12 weeks - In hyperemesis gravidarum, the hCG levels are often higher and extend beyond the first trimester - Endocrine theory- high levels of hCG and estrogen during pregnancy - Metabolic theory- vitamin B6 deficiency - Psychological theory- psychological stress increases the symptoms - Therapeutic Management - Conservative management in the home is the first line of treatment for the woman with hyperemesis gravidarum - Usually focuses on dietary and lifestyle changes - On admission to the hospital, blood tests are ordered to assess the severity of the client’s dehydration, electrolyte imbalance, ketosis, and malnutrition - Parenteral fluids and drugs are ordered to rehydrate and reduce symptoms - If the client does not improve after several days of bed rest, “ gut rest”, IV fluids, and antiemetics, total parenteral nutrition or feeding through a percutaneous endoscopic gastrostomy tube is initiated to prevent malnutrition - Administering antiemetics IV or IM is typically the second pillar of treatment for hyperemesis gravidarum - Medication used for Hyperemesis Gravidarum include: - Promethazine - Prochlorperazine - Ondansetron - Laboratory and Diagnostic Testing - - Liver enzyme: to rule out hepatitis, pancreatitis, and cholestasis; elevations of aspartate aminotransferase (AST) and alanine aminotransferase (ALT) ar usually present - CBC- elevated levels of RBC and hematocrit, indicating dehydration - TSH and T4 to rule out thyroid disease - BUN- increased in the prescenese of salt and water depletion - Urine Specific Gravity- greater than 1.025, possibly indicating concentrated urine linked to inadequate fluid intake or excessive fluid loss; ketonuria - Serum electrolytes- decreased levels of potassium, sodium, and chloride resulting from excessive vomiting and loss of HCL acid in stomach Promoting Comfort and Nutrition - During the initial period, expect to withhold all oral food and fluids maintaining NPO status to allow the GI tract to rest - Administer prescribed antiemetics to relieve the nausea and vomiting and IV fluids to replace fluid losses - Administer electrolyte replacement therapy as ordered to correct any imbalances and periodically check serum electrolyte levels to evaluate the effectiveness of therapy - - - - - - - - TISSUE INTEGRITY Perineal lacerations or tears can occur during the second stage when the fetal head emerges through the vaginal introitus. Extent of laceration is defined by depth: - 1st degree: extends through the skin - 2nd degree: extends through the muscles of the perineal body - 3rd degree: laceration that continues through the anal sphinceter muscle - 4th degree: laceration also involves the anterior rectal wall ● Special attention needs to be paid to third and fourth degree lacerations to prevent fecal incontinence Risks for third or fourth degree lacerations included mulliparity, being Asian or Pacific Islander, increased birth weight of newborn, operative vaginal birth, episiotomy, and longer second stage of labor Episiotomy: an incision made in the perineum to enlarge the vaginal outlet and theoretically to shorten the second stage of labor - Midline episiotomy has been the most commonly used one in the United States because it can be easily repaired and causes the least of pain The perineum is often edematous and bruised for the first day or two after birth. If the birth involved an episiotomy or laceration, complete healing may take as long as 4-6 months in the absence of complications at the site, such as hematoma or infection. Perineal lacerations may extend into the anus and cause considerable discomfort for the mother when she is attempting to defecate or ambulate Often women are hesitant to have a bowel movement due to pain in the perineal area resulting from an episiotomy, lacerations, or hemorrhoids. - Stool softeners and/or laxatives used to treat constipation have been prescribed for them to reduce discomfort During the early postpartum period, the perineal tissue surrounding the episiotomy site is typically edematous and slightly bruised. The normal episiotomy site should not have redness, discharge, or edema. The majority of healing takes place within the first 2 weeks, but it may take 4-6 months for the episiotomy to completely heal Assess the episiotomy and any lacerations at least every 8 hours to detect hematomas or signs of infection. - Larger areas of swollen, bluish kin with complaints with complaints of severe pain in the perineal area indicate pelvic or vulvar hematomas - A white line running the length of the episiotomy is a sign of infection, as well as swelling or discharge. - Severe intractable pain, perineal discoloration, and ecchymosis indicates a perineal hematoma, a potentially dangerous condition Ice can be applied to relieve discomfort and reduce edema; sitz baths also can promote comfort and perineal healing - - The acronym REEDA is frequently used for assessing a woman’s perineum status. It is derived from five components that have been identified to be associated with the healing process of the perineum. These include: - 1. Redness—area may also feel warm to touch. - 2. Edema—may indicate infection or a hematoma. - 3. Ecchymosis—may indicate vaginal trauma. - 4. Discharge—should follow the expected lochia pattern. - 5. Approximation of skin edges—should be well aligned without gaps. - Each category is assessed and a number assigned (0 to 3 points) for a total REEDA score ranging from 0 to 15 Postpartum infection is defined as a fever of 100.4° F (38° C) or higher after the first 24 hours after childbirth, occurring on at least 2 of the first 10 days after birth, exclusive of the first 24 hours


![[Physician Letterhead] [Select Today`s Date] . [Name of Health](http://s3.studylib.net/store/data/006995683_1-fc7d457c4956a00b3a5595efa89b67b0-300x300.png)