Hyper Type III
advertisement
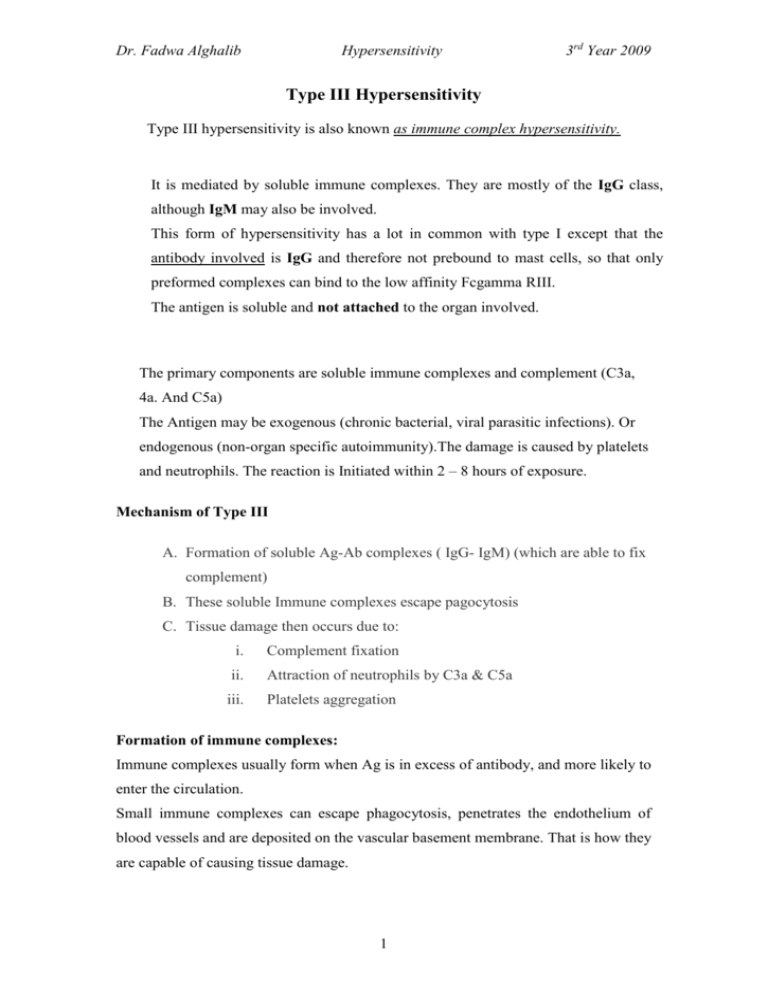
Dr. Fadwa Alghalib Hypersensitivity 3rd Year 2009 Type III Hypersensitivity Type III hypersensitivity is also known as immune complex hypersensitivity. It is mediated by soluble immune complexes. They are mostly of the IgG class, although IgM may also be involved. This form of hypersensitivity has a lot in common with type I except that the antibody involved is IgG and therefore not prebound to mast cells, so that only preformed complexes can bind to the low affinity Fcgamma RIII. The antigen is soluble and not attached to the organ involved. The primary components are soluble immune complexes and complement (C3a, 4a. And C5a) The Antigen may be exogenous (chronic bacterial, viral parasitic infections). Or endogenous (non-organ specific autoimmunity).The damage is caused by platelets and neutrophils. The reaction is Initiated within 2 – 8 hours of exposure. Mechanism of Type III A. Formation of soluble Ag-Ab complexes ( IgG- IgM) (which are able to fix complement) B. These soluble Immune complexes escape pagocytosis C. Tissue damage then occurs due to: i. Complement fixation ii. Attraction of neutrophils by C3a & C5a iii. Platelets aggregation Formation of immune complexes: Immune complexes usually form when Ag is in excess of antibody, and more likely to enter the circulation. Small immune complexes can escape phagocytosis, penetrates the endothelium of blood vessels and are deposited on the vascular basement membrane. That is how they are capable of causing tissue damage. 1 Dr. Fadwa Alghalib Hypersensitivity 3rd Year 2009 Mechanism of Tissue Damage: 1) Large quantities of soluble antigen-antibody complexes form in the blood and are not completely removed by macrophages. 2) These antigen-antibody complexes lodge in the capillaries between the endothelial cells and the basement membrane. 3) The antigen-antibody complexes activate the classical complement pathway and complement proteins and antigen-antibody complexes attract leukocytes to the area. 4) The leukocytes then discharge their killing agents and promote massive inflammation. This leads to tissue death and hemorrhage. Deposition of immune complexes (IC) in blood vessels Vascular permeability IC deposit in blood vessel wall Induce platelet aggregation and complement activation Platelets form microthrombi on basement membrane Neutrophils are attracted Fail to ingest the complexes Release their lysosomal enzymes Causing further damage to vessel wall There are 3 examples of type III reactions: 1. Arthus reaction (Local Deposition) 2. Serum sickness (Generalized Deposition) 3. Immune complex disease i. auto immune disease ii. Glomerulonephritis iii. pneumonitis Mechanism of Immune-Complex Deposition: 1) Local Deposition--- Arthus Reaction: Immune complexes are deposited in vessel walls. These complexes are due to receiving high amounts of antigen, which cause huge amounts of antibodies to be 2 Dr. Fadwa Alghalib Hypersensitivity 3rd Year 2009 produced, then receiving the antigen subcutaneously. This causes edema and hemorrhage. Repeated subcutanious injection of an Ag results in local formation of immune complexes. Erythema, oedema and necrosis due to accumulation of neutrophils. E.g: rabies vaccine, insulin injection Development of Arthus reaction.: Exposure to an antigen > immune complex (Ag-Ab) formation > complement activation (C3a, C4a, and C5a,) > release of small complement subunits > C5a induce mast cell degranulation, chemotaxis of neutrophils > lytic enzyme release during neutrophil attempts at phagocytosis. 2) Generalized Deposition---- Serum Sickness: This term originated when serum from immunized animals was used to treat diphtheria and tetanus. immune complexes form and circulate or precipitate. They cause fever, itching, arthralgia, arthritis, lymphadenopathy, and splenomegaly. Develops after 7-10 days from first exposure within 2-3days for secondary immune response. 3- Immune complex diseases They are three groups: 1. Persistent infections 2. Autoimmune diseases 3. Inhalation of antigenic material a- Persistent Infections: continued infection and continual production of antigen & plasma cells continue producing Abs. Immune complexes continually generated Deposition of Immune complexes Stimulate inflammation E.g. Poststreptococcal glomerulonephritis (PSGN), (streptococci, some viruses (Chronic Viral Hepatitis), malaria) 3 Dr. Fadwa Alghalib Hypersensitivity 3rd Year 2009 b- Autoimmune diseases A. Continued production of Autoantibody to a self-antigen B. Leads to prolonged immune complex formation E.g: 1. Rheumatoid arthritis (RA is an autoimmune disorder that causes joint inflammation). 2. SLE: Accumulation of DNA complexed with anti-DNA Ab in synovial membranes or kidney basement membranes yielding arthritic symptoms or kidney damage. 3. hyperthyroidism is occasionally caused by long acting thyroid stimulators (LATS) as a result of an autoimmune reaction. c- Inhalation of antigenic material 1. Some common inhaled Ags provoke IgG rather than IgE response Type III 2. Repeated inhalation of hay dust, mold, spores, formation of immune complexes deposit in lungs E.g: Farmer’s Lung Disease Diagnosis : Detection of immune Complexes: 1) In Tissues Tissue biopsies for deposits of Ig and complement by immunofluorescence 2) In Serum A- Measurement of serum level of C3 and C4 ( usually decreased) 4