Hemolytic Anemias-Combined
advertisement
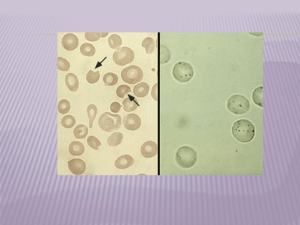
Sickle Cell Anemia (Hemoglobinopathies) By: Jessica Hebert, Rob McElroy, Beth McQuinn, Yuway Tsing, Elias Kass, Bill Walter, Amelia Kramer What are hemolytic anemias? • Decreased life-span of erythrocytes • Removal of RBCs may be: – Intravascular (within the blood) – Extravascular (within the spleen) • Associated with: – Increased erythropoiesis – Increased hemoglobin catabolism byproducts Possibilities? • Many types of hemolytic anemias: – G6PD-Deficiency – Hemoglobinopathies • Sickle Cell Disease • Hereditary Spherocytosis • Thalassemias – Immunohemolysis – Others… Background: Prevalence in Populations Population Prevalence African American 1/375 HbSS , 1/835 HbSC , 1/10 HbSA (trait) American > 50,000 (2 mil with sickle cell trait) Mediterranean descent significant Caribbean descent Not significant East Indian Ancestry Not significant Arabian Not significant Latin American 1/1000-1400 Greeks Not significant Italians Not significant •http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Search&db=books&doptcmdl=GenBookHL&term=sickle+cell+prevalence+AND+ hstat%5Bbook%5D+AND+340265%5Buid%5D&rid=hstat6.section.17004 Clinical Presentation: Signs and Symptoms General anemia pallor, fatigue, SOB on exertion Acute chest syndrome cough, dyspnea, chest pain, fever Infection malaise, cough and chest pain, diarrhea and/or vomiting Painful crises persistent pain in skeleton, chest, and/or abdomen Hand-foot syndrome swollen and painful hands and feet (by 2 years of age: 50% of Jamaican and 25% of American children with sickle cell anemia have experienced at least one episode of dactylitis) Stroke (affects 10% of patients; 6-17% of children and young adults), sudden neurologic deficits including motor, difficulty with language, writing, and/or reading; seizures; sensory deficits; altered consciousness Priapism penile erection not related to arousal Delayed growth and puberty Patient more slender or small in size. Jaundice Yellowing of skin and eyes Other Some people remain asymptomatic into late childhood and are only incidentally diagnosed http://www.ornl.gov/sci/techresources/Human_Genome/posters/chromosome/sca.shtml Background Clinical Presentation • There are a range of Treatments per extremes or per symptoms Sickle Cell Anemia A hereditary genetic disorder that results in the production of abnormal hemoglobins In Sickle Cell, the Beta chain is affected by a point mutation… Source: Robbins One small point mutation leads to a major problem when HbS is deoxygenated… Deoxyhemoglobin A (HbA) Deoxyhemoglobin S (HbS) http://www.ornl.gov/sci/techresources/Human_Genome/posters/chromosome/hbb.shtml A prolonged environment of low oxygen leads to aggregation and polymerization of hemoglobins into long chains of rod-like fibers, causing the RBC to form the shape of a crescent or sickle. • Donut-shaped • Soft and malleable • Able to pass through small spaces • Lifespan ~120 days • Sickle-shaped • Hard and rod-like • Gets stuck in narrow spaces • Lifespan ~20 days http://www.humanillnesses.com/original/images/hdc_0001_0003_0_img0235.jpg Sickling of red blood cells leads to: 1. Vaso-occlusive complications 2. Severe anemia 3. Chronic hyperbilirubinemia Vaso-occlusive complications Occur in areas with: • Prolonged, low oxygen tension • Decreased pH • Inflammation • Low blood flow Source: Robbins Severe Anemia and Chronic Hyperbilirubinemia 1. Young RBCs with HbS can alternate between the sickled and normal formation. 2. However, sickling causes oxidative damage to the RBCs cell membrane (and to the cells around it). 3. Eventually, RBCs become irreversibly sickled. Severe Anemia and Chronic Hyperbilirubinemia • Irreversibly sickled cells end up in the spleen. • Hemolysis occurs at the splenic cords. • Decreased RBCs and increased bilirubin • Infarction and fibrosis causes autosplenectomy. Source: Robbins G6PD-Deficiency Distribution G6PD-Deficiency Distribution • 12% of males of African descent (A type) • 22% of Southeast Asian males (Mahedian type) • 50% of Kurdish males (Mediterranean type) • Also, a significant prevalence in males of Italian, Greek, Lebanese, Iraqi, and Sephardic heritage (Mediterranean type) G6PD-Deficiency Presenting Symptoms • Fatigue or muscle weakness • Jaundice or pallor • Dyspnea • Dark urine • Pain (especially abdominal) • Splenomegaly Glucose 6-Phosphate G6PD-Deficiency – Pathology • Genetic abnormalities (of which there are several varieties) lead to deficient or impaired enzyme function • High levels of oxidants (from foods, drugs, exercise, infections) may damage or denature proteins within the erythrocyte • RBCs may then be subject to intravascular or extravascular hemolysis G6PD Crisis Precipitation - Beans • Broad beans (favism) – Fava beans, bell beans, fever beans, hava beans, pigeon beans, horse beans, tick beans, silkworm beans, English dwarf beans G6PD Crisis Precipitation Oxidizing Drugs – Antimalarials (primaquine, quinine, quinidine) – NSAIDs (aspirin, ibuprofen) – Antibiotics (sulfonamides) – Nitrofurantoin – TCM herbs (rhizoma coptidis, margarita, calculus bovis) Other oxidants – Henna – primarily infants and pregnant women – Naphthlene (moth balls) – regular exposure Early Lab Tests – CBC • • • • • • • RBC – Low Hct – Low Hb – Low MCV – Normal to High MCHC – Low to Normal MCH – Low to Normal So…initial CBC is only your starting point Early Lab Tests – Urinalysis • Hemoglobin – Elevated post-crisis • Bilirubin – Elevated post-crisis • Urobilinogen – Elevated post-crisis • May also see hematuria, proteinuria, LDH • These account for dark color of urine following a crisis, but are also non-specific for any given type of hemolytic anemia Early Lab Tests - Smear • Often readily seen with initial CBC, or easily ordered alongside • If anemias are suspected, probably best to run a smear in the early stages • G6PD-Deficiency may show: – Heinz bodies • Denatured Hb bound to cell membrane • May damage cell membrane, leading to intravascular hemolysis – “Bite” cells • Spleen removes portion of RBC that had Heinz body, preventing intravascular hemolysis – These aren’t typically present immediately following an acute hemolytic crisis (problem cells have been destroyed) Other Non-Specific Lab Tests • Reticulocyte count – – – – May be elevated following acute crisis (6-8 weeks) May be normal in non-crisis situations May be reduced in aplastic crisis (could go to zero) Should be considered in conjunction with smear, other data • Serum bilirubin – Present in the unconjugated (prehepatic) form – Elevated after an acute hemolytic crisis • Serum haptoglobin – Binds to Hb in the blood for removal by spleen (preventing Hb from excretion in the urine, which could lead to renal failure) – Decreased (depleted) after an acute hemolytic crisis Screening for G6PD • Cells from G6PD-deficient subjects can’t convert the oxidized substrate to a reduced state • Different tests use different substrates • Substrates can either be the enzyme’s natural substrate (NADP) or substrates from secondary reactions Fluorescent Screening Test • G6PD generates NADPH • NADPH fluoresces under long-wave UV light • No G6PD? No fluorescence. Fluorescent Screening Test • Shortcomings: – False Negative: young red blood cells have more G6PD activity. During an acute hemolytic episode, reticulocytosis results in a bigger population of young red blood cells, so even in G6PD Deficiency, the fluorescence may appear normal. – False Positive: if the patient is anemic, very little fluorescence may be seen because there are very few red blood cells. Methemoglobin Reduction Test • Sodium nitrite converts Hb (hemoglobin) to Hi (methemoglobin) • Adding methylene blue should stimulate the pentose phosphate pathway, reducing methemoglobin • In G6PD Deficiency, methemoglobin persists Methemoglobin Reduction Test • Normal blood → clear red color • Deficient blood → brown color • Heterozygotes → intermediate color Methemoglobin Reduction Test - Takes longer than fluorescence + Extremely inexpensive + Requires only a water bath • Test should be complemented by cytochemical analysis Cytochemical Analysis • Only way to reliably detect deficiency in heterozygous women • More reliable than assay • Good complement for other tests Cytochemical Analysis • Treat red cells to convert their oxyhemoglobin (HbO2) to methemoglobin (Hi) • In the presence of G6PD, Hi converts back to HbO2 • Add MTT, which will be reduced by HbO2 to an insoluble form • In G6PD Deficiency: – Hi persists – MTT is not reduced – Ergo, cells are not stained Cytochemical Analysis Cytochemical Analysis • Interpretation: – Normal G6PD activity: majority stained – Hemizygous: majority unstained – Heterozygotes: • Most show mosaicism (40-60% unstained) • Some have only 2-3% unstained (fortunate lyonization) G6PD Assay • Tracks activity of enzyme by following rate of production of NADPH over time • NADPH has peak of UV light absorption at 340nm • Note potentially misleading results in following table G6PD Assay Ma le Fem a le In he a lth In in creas e d de mo ly s is u n relate d t o G6P D defi ci en c y Dur in g rec o ve ry f ro m G6P D- re lat e d an e m ia Gd + (n orm al) Gd ( e nti rely defici e nt ) Gd+/ Gd + ( norm al) Gd -/ Gd( e nti rely defici e nt ) Gd+/ Gd ( so m e what deficie nt) 7 -1 0 <2 2 -7 15 4 4 -9 6.5 ( a p pe ar s norm al) 6 -1 0 ( a p pe a rs norm al) Values are examples only (Lewis 10e, p226) G6PD Assay • Interpretation: – Red cells are likely to lyse from G6PD deficiency if they have less than ~20% of normal enzyme activity • Confounding factors: – With reticulocytosis, the relatively large population of reticulocytes yields a higher enzyme activity, covering up deficiency – Therefore, a low-normal enzyme activity assay during reticulocytosis points towards G6PD deficiency (without deficiency, values would be very high during reticulocytosis) – Re-evaluate after reticulocytosis slows Choosing Appropriate Tests • More than one test should be used • Are they in the middle of a hemolytic crisis? – Anemia + Reticulocytosis = Misleading results • For females, cytochemical analysis should be used • Normal and deficient control blood should always be used for comparison – Sheep are naturally deficient, bah!