G6PD

Glucose 6-phosphate dehydrogenase deficiency
HMIM224
Objectives of the Lecture
1- Understanding the main functional concepts for pentose phosphate pathway (also called hexose monophosphate pathway).
2- Identify the main general uses of NADPH for normal cellular metabolism with special focus on its rule for antioxidant mechanisms.
3- Describing the genetic & biochemical basis of glucose 6 phosphate dehydrogenase deficiency (G6PD deficiency) with identifying its clinical implication in causing hemolytic anemia.
4- Recognizing the precipitating factors for G6PD deficiency anemia
5- Recalling classes of G6PD deficiency anemia ( as indicated by variants of G6P dehydrogenase enzyme)
6- Discussing the biochemical & clinical rationale for lines of diagnosis of G6PD deficiency anemia.
Pentose Phosphate Pathway (PPP)
or Hexose Monophosphate Pathway (HMP)
Pentose Phosphate Pathway (PPP) or Hexose monophosphate pathway (HMP):
- is an alternative oxidative pathway for glucose rather glycolysis
- results in no ATP production (not like glycolysis)
- is the major pathway for NADPH production
- produces ribose-5-phosphate for nucleotide synthesis (required for DNA, RNA & others)
-
AEROBIC VS ANAEROBIC GLYCOLYSIS
Pentose Phosphate Pathway (PPP) or Hexose Monophosphate Pathway (HMP)
as a source for NADPH
2 NADPH are produced for each one molecule of glucose
Glucose
Glucose 6-phsphate
Dehydrogenase
First enzyme in the pathway
Pentose phosphate pathway (or hexose monophosphate pathway) occurs in the cytosol of many cells of the body including RBCs.
Pentose Phosphate
Pathway (PPP
)
Glucose-6-phosphate dehydrogenase
Uses of NADPH in normal cellular metabolism
1- Role in fatty acid synthesis (reductive agent)
2- Role in antioxidant mechanisms (part of glutathione system)
3- Role in oxygen-dependent phagocytosis by WBCs
4- Role in synthesis of nitric oxide (NO)
Role of NADPH in antioxidant mechanisms
Introduction
Hydrogen peroxide (H
2
O
2
) is one member of the family of reactive oxygen species (ROS).
Reactive oxygen species (ROS) are formed from partial reduction of molecular O
2 i.e. adding electrons to oxygen leading to the formation of superoxide, hydrogen peroxide and hydroxyl radical.
ROS are formed continuously from aerobic metabolism of drugs and environmental toxins
or diminished antioxidants. All these lead to oxidative stress.
ROS cause damage to DNA, protein and unsaturated lipids of the cells including cell membranes..
They are implicated in cancer, chronic inflammatory disease and aging.
Role of NADPH in antioxidant mechanisms
(cont.)
Introduction
(cont.)
:
The cell has different protective mechanisms that serve to minimize the toxic potential of
ROS (antioxidant effect) as follows:
A) Enzymes that catalyze antioxidant reactions :
i- Catalase & superoxide dismutase enzymes catalyze the conversion of the toxic ROS to harmless products.
ii- Glutathione reductase reduces oxidized glutathione to reduced glutathione
B) Antioxidant chemicals :
Vitamins E, C and b -carotene (precursor of vitamin A) reduce ROS .
Reactive Oxygen Species (ROS)
Role of NADPH in antioxidant mechanisms
(cont.)
Reduced Glutathione :
Introduction
(cont.) :
Reduced Glutathione (G-SH) reduces hydrogen peroxide (H
2
O
2
) into oxidized glutathione (G-S-S-G) and water. The reaction is catalyzed by glutathione peroxidase
Oxidized glutathione is reduced to reduced glutathione by glutathione reductase using NADPH as a source of reducing equivalents.
Reduced glutathione
•
Oxidized glutathione
Glucose 6-phosphate dehydrogenase deficiency
(G6PD deficiency)
Definition
• It is an inherited disease characterized by hemolytic anemia caused by inability to detoxify oxidized agents.
• G6PD deficiency is the most common disease producing enzyme anomalies in humans, affecting more than 200 million individuals worldwide.
The highest prevalence in the Middle East, tropical Africa & Asia.
• G6PD Deficiency is caused by 400 different mutations in gene coding for
G6PD, only few of them causes the clinical symptoms of the disease.
Mode of inheritance of G6PD Deficiency
• It is X- linked recessive genetic disorder (gene is carried on X-chromosome).
• The gene is present on the X chromosome
• The inheritance follows specific pattern:
Males have one X chromosome
So, they will be diseased if they have the affected gene ( x Y)
Females have 2 X chromosomes may be homozygous or heterozygous
Homozygous: are diseased ( xx )
Heterozygous: are not diseased BUT: carriers (X x )
& can transfer the disease to their sons
Normal
Father
(XY)
X
Normal
Heterozygous (carrier)
Mother
( X x )
• x X
X x XX
50% of
Daughters are normal carriers
50% of
Sons are affected
Y Y x YX
Punnet Square for X-linked Recessive Inheritance
Decreased amounts of reduced glutathione due to decreased production of NADPH
Reduction of amounts of NADPH in RBCs in G6PD deficiency causes decrease in reduction of oxidized glutathione to reduced glutathione.
Role of reduced glutathione in RBCs:
1- Reduced glutathione gets rid of ROS including hydrogen peroxide.
2- Reduced Glutathione helps to keep sulfhydryl groups of hemoglobin protein in the reduced state.
Decreased amounts of reduced glutathione due to decreased production of NADPH
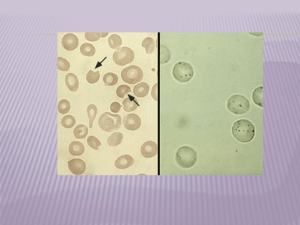
Reduction of production of reduced glutathione results in:
1- A decrease in detoxication of peroixides. This causes damage to RBCs membrane and hemolysis (ending in hemolytic anemia ).
2- Hemoglobin protein is denatured forming insoluble masses (Heinz bodies). Heinz bodies attach to red cell membranes.
Membrane proteins are also oxidized.
Accordingly, red cells become rigid and removed from the circulation by macrophages in the spleen and liver ending in anemia
Decreased amounts of reduced glutathione due to decreased production of NADPH
Deficiency of G6PD occurs in all cells of affected individual.
It is severe in RBCs because the only pathway to form NADPH in RBCs is
pentose phosphate pathway (using G6PD).
Precipitating factors in G6PD deficiency:
• Individuals who have inherited one of the many G6PD mutations do not show clinical manifestation.
• Some of patients with G6PD develop hemolytic anemia if they are exposed or ingest any of the followings oxidizing agents:
1-Oxidant drugs:
Antibiotics : e.g. sulfamethoxazole
Antimalarias : e.g. primaquine
Antipyretics : e.g. acetanilid
2- Favism:
The hemolytic effect of ingesting of fava beans is not observed in all individuals with G6PD deficiency but all patients with favism have G6PD deficiency
G6PD Variants
• Most G6PD variants are caused by point mutations in the G6PD gene.
• Some of these point mutations do not disturb the structure of the enzyme's active site and hence, do not affect enzyme activity.
• Other point mutations may lead to production of mutant enzymes with one or more of the following : altered catalytic activity, decrease stability an alteration of binding affinity for NADP + or Glucose 6-phosphate.
• The severity of diseases usually correlates with the amount of residual enzyme activity in the patient’s red cells.
G6PD Variants
G6PD Variants can be classified into :
Class III (G6PD Group A ) :
A moderate form of the disease
RBCs contain unstable G6PD enzyme, but normal activity in younger RBCs and reticulocytes.
Accordingly, only older RBCs are hemolysed in a hemolytic episode.
Class II mutations (G6PD Mediterranean):
More severe
G6PD enzyme shows normal stability but, very low activity in all RBCs.
Class I mutations:
It is often associated with chronic non spherocytic anaemia
(occurs even in absence of oxidative stress).
G6PD Variants
• Both G6PD Mediterranean and G6PD A- represent mutant enzymes that differ from the normal variants by a single amino acid. This change is due to DNA changes in the form of point mutations or missense mutations.
• Frame shift mutations or large deletions have not been identified indicating that the complete absence of G6PD is lethal.
• Mutation causing non spherocytic hemolytic anemia are clustered near the carboxyl end of the enzyme, whereas mutations causing milder forms of the disease tend to be located at the amino end of the enzyme.
Diagnosis of
G6PD Deficiency Hemolytic Anemia
•
• Diagnosis of hemolytic anemia
CBC and reticulocytic count
•
•
• Screening:
Qualitative assessment of G6PD enzymatic activity
(UV-based test)
•
• Confirmatory test:
Quantitative measurement of G6PD enzymatic activity
•
• Molecular test:
Detection of G6PD gene mutation
Reference
• Lippincott’s Illustrated Biochemistry
• Essential Hematology(Hoffbrand, Pettit & Moss)