Patient
advertisement
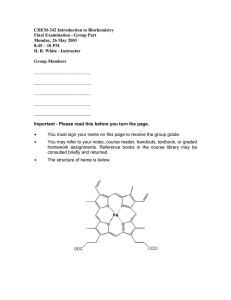
Building Blocks of Life Clinical Case Presentation #4 Glucose 6 Phosphate Dehydrogenase Deficiency Template for a Clinical Case Presentation •Chief Complaint (CC) •History of Chief Complaint (HCC) •Medications (Meds) •Social History (SH) •Family History (FH) •Dental History (DH) •Past Medical History (PMH) •Review of Systems (ROS) •Diagnosis -Risk Assessment (DRA) •Differential Diagnosis (DDx) •Treatment (Tx) •Prognosis (PR) Test at the end of this presentation! So pay ATTENTION! Clinical presentation Patient • 48 year old male who recently planned a trip to India • Chief Complaint (CC) • Weakness, fatigue and dark urine • History of Chief Complaint (HCC) • One month • Medications • Primaquine, aspirin • Social History (SH) • ETOH socially, denies recreational use of any nonprescription meds. • Family History (FH) • Uncle who c/o “bleeding problem” during WWII in the Pacific campaign •Dental History (DH) •Excellent oral hygiene. Last check up 2months ago. •Medical History (MH) • No significant medical history, with the exception of a tonsillectomy at age 6. • Review of Systems (ROS) • Cardiovascular – Blood Pressure, 120/80 , Pulse 96 irregular. • Respiratory – Rate 18/min. SOB • Nervous – Dizziness • Endocrine – WNL • Renal – dark, cloudy urine • Gastrointestinal – occasional dyspepsia • Skin and mucosa – Color and texture of skin slightly jaundiced • Osteoarticular – WNL •Eyes- yellow sclera Diagnosis and Risk Assessment Are there any contributing factors as per the medical history? 1. 2. 3. 4. 5. 6. 7. Medications Family history Recent travel Immunizations Fatigue Dark urine Yellow sclera Dietary Questionnaire What if any foods would contribute to this? •Eats spicy foods, on occasion. •Drinks wine •Eats red meat and chicken 3/wk •Vegetables, fava beans . Pathogenesis of G6PD Deficiency The Hexose Monophosphate Shunt Hexokinase GLUCOSE 6 Phosphate GLUCOSE NADPH+ ATP ADP G6PD NADPH Glutathione reductase GSSG 6 phosphogluconate GSH Diagnosis of G6PD Deficiency • • • • • • G6PD assay Urinalysis Genetic test Family history Laboratory values Hct/Hgb Dietary history Differential Diagnosis • Bone marrow infiltration from lymphoma, carcinoma • Severe infection • Drug toxicity • Iron deficiency anemia • Autoimmune disease Treatment and Prognosis Etiologic and symptomatic treatment • No specific treatment is needed, condition is usually self limiting • Symptomatic treatment •Rarely blood transfusions are indicated •Adequate urine output should be insured Prognosis •Severe cases may be life threatening •Avoid causative agents Answer the following • What is foods or medications should patients avoid? • What test(s) are used to diagnose G6PDD? • What treatment can be instituted? • What are the differential diagnoses of G6PDD? • What chromosome is associated with G6PDD? Thank You