IMMUNOMODULATORS
advertisement

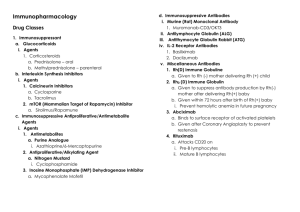
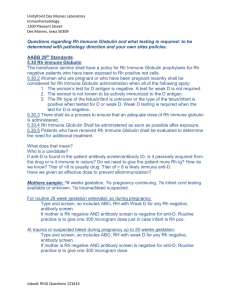
IMMUNOMODULATORS Prof. Mervat Hesham The Immune Response - why and how ? Discriminate: Self / Non self Destroy: Infectious invaders Dysregulated self (cancers) Immunity: Innate, Natural Adaptive, Learned • Innate immune response – first line of defense against an antigenic insult. Includes defenses like physical (skin), Biochemical (complement, lysozyme, interferons) cellular components (neutrophils, monocytes, macrophages). • Adaptive immune response a) Humoral immunity - Antibody production – killing extracellular organisms. b) Cell mediated immunity – cytotoxic / killer T cells – killing virus and tumour cells. Who are involved ? Innate Complement Granulocytes Adaptive: B and T lymphocytes Monocytes/macroph B: antibodies ages T : helper, NK cells cytolytic, suppressor. Mast cells Basophils ABNORMAL IMMUNE RESPONSE • Hypersensitivity reactions Type 1 – Anaphylactic shock Type 2 – mismatched blood transfusion Type 3 – Serum Sickness, glomerulonephritis and arthritis. Type 4 – TB, leishmaniasis. Autoimmunity – Autoimmune diseases arise when the body mounts an immune response against itself as a result of failure to distinguish self tissues and cells from foreign antigens. Rheumatoid Arthritis, S.L.E, Type 1 Diabetes Mellitus, Multiple Sclerosis etc…. • Immunodeficiency Diseases a) Congenital – Di George’s syndrome, SCID due to ADA deficiency. b) Extrinsic – HIV causing AIDS. IMMUNOMODULATORS DEFINITION Immunomodulators are drugs which either suppress the immune system – Immunosuppressants or stimulate the immune system – Immunostimulants immunosuppressant Immunosuppressants Glucocorticoids - Prednisolone. Calcineurin inhibitors Cyclosporine Tacrolimus Antiproliferative / antimetabolic agents Sirolimus Everolimus Azathioprine Mycophenolate Mofetil Others – methotrexate, cyclophosphamide, thalidomide and chlorambucil , Interferon Antibodies Antithymocyte globulin Anti CD3 monoclonal antibody Muromonab Anti IL-2 receptor antibody – Daclizumab, basiliximab Anti TNF alpha – infliximab, etanercept Immunosuppressants Organ transplantation Autoimmune diseases Problem Life long use Infection, cancers Nephrotoxicity Diabetogenic Glucocorticoids Induce redistribution of lymphocytes – decrease in peripheral blood lymphocyte counts Intracellular receptors – regulate gene transcription Down regulation of IL-1, IL-6 Inhibition of T cell proliferation Neutrophils, Monocytes display poor chemotaxis Broad anti-inflammatory effects on multiple components of cellular immunity USES - Glucocorticoids Transplant rejection GVH – BM transplantation Autoimmune diseases – RA, SLE, Hematological conditions Psoriasis Inflammatory Bowel Disease, Eye conditions Toxicity Growth retardation Avascular Necrosis of Bone Risk of Infection Poor wound healing Cataract Hyperglycemia Hypertension CALCINEURIN INHIBITORS • Calcineurin (CN) is a protein phosphatase activates the T cells of the immune system and can be blocked by drugs. Cyclosporine – – bind to the cytosolic protein cyclophilin (an immunophilin) of immunocompetent lymphocytes, especially T-lymphocytes. This complex of ciclosporin and cyclophilin inhibits the phosphatase calcineurin, which under normal circumstances induces the transcription of interleukin-2. The drug also inhibits lymphokine production and interleukin release, leading to a reduced function of effector T-cells. Uses Organ transplantation: Kidney, Liver, Heart Rheumatoid arthritis, IBD, uveitis Psoriasis Aplastic anemia Skin Conditions- Atopic dermatitis, Alopecia Areata, Pemphigus vulgaris, Lichen planus, Pyoderma gangrenosum Toxicity : Cyclosporine Renal dysfunction Tremor Hirsuitism Hypertension Hyperlipidemia Gum hyperplasia Hyperuricemia – worsens gout Calcineurin inhibitors + Glucocorticoids = Diabetogenic Tacrolimus ( FK 506, Prograf ) – It binds to the immunophilin FKBP1A, followed by the binding of the complex to calcineurin and the inhibition of its phosphatase activity. In this way, it prevents the cell from transitioning from the G0 into G1 phase of the cell cycle. Tacrolimus is more potent than ciclosporin and has less pronounced side-effects. Use -Prophylaxis of solid-organ allograft rejection –Topical preparation available for use in atopic dermatitis and psoriasis. Toxicity - Tacrolimus Nephrotoxicity Neurotoxicity-Tremor, headache, motor disturbances, seizures GI Complaints Hypertension Hyperglycemia Risk of tumors, infections Sirolimus (rapamycin, trade name Rapamune) Contrary to ciclosporin and tacrolimus, drugs that affect the first phase of T lymphocyte activation, sirolimus affects the second one( namely signal transduction and lymphocyte clonal proliferation). It binds to FKBP1A like tacrolimus, however the complex does not inhibit calcineurin but another protein, mTOR (mammalian target of rapamycin ). It indirectly inhibits several T lymphocyte- specific kinases and phosphatases, hence preventing their transition from G1 to S phase of the cell cycle. Sirolimus prevents B cell differentiation into plasma cells, reducing production of IgM, IgG, and IgA antibodies. CELL CYCLE Sirolimus Uses Prophylaxis of organ transplant rejection with other drugs Toxicity Increase in serum cholesterol, Triglycerides Anemia Thrombocytopenia Hypokalemia Fever GI effects Risk of infection, tumors Azathioprine (Imuran ) the main immunosuppressive cytotoxic substance. It is nonenzymatically cleaved to mercaptopurine, that acts as a purine analogue and an inhibitor of DNA synthesis. By preventing the clonal expansion of lymphocytes in the induction phase of the immune response, it affects both the cell and the humoral immunity. Uses Prevention of organ transplant rejection Rheumatoid arthritis Toxicity - Azathioprine Bone marrow suppression- leukopenia, thrombocytopenia, anemia Increased susceptibility to infection Hepatotoxicity Alopecia GI toxicity Drug interaction: Allopurinol Mycophenolate Mofetil Prodrug Mycophenolic acid Inhibits IMPDH – enzyme in guanine synthesis (Inosine monophosphate dehydrogenase (IMPDH) is a major target for both antitumor and immunosuppresive drug design.) T, B cells are highly dependent on this pathway for cell proliferation Selectively inhibits lymphocyte proliferation, function , Antibody formation, cellular adhesion, migration Uses - Mycophenolate Mofetil Prophylaxis of transplant rejection Combination: Glucocorticoids Calcineurin Inhibitors Toxicity GI, Hematological Diarrhea, Leucopenia Risk of Infection Drug Interaction Decreased absorption when co- administered with antacids Acyclovir, Gancyclovir compete with mycophenolate for tubular secretion Antibodies Against lymphocyte cell-surface antigens Polyclonal / Monoclonal Antibodies Antithymocyte Globulin Monoclonal antibodies Anti-CD3 Monoclonal antibody (Muromonab-CD3) Anti-IL-2 Receptor antibody (Daclizumab, Basiliximab) Campath-1H (Alemtuzumab) Anti-TNF Agents Infliximab Etanercept Adalimumab LFA-1 Inhibitor (lymphocyte function associated) Efalizumab Anti-thymocyte Globulin Purified gamma globulin from serum of rabbits immunized with human thymocytes Cytotoxic to lymphocytes & block lymphocyte function Uses Induction of immunosuppression – transplantation Treatment of acute transplant rejection Toxicity Hypersensitivity Risk of infection, Malignancy Anti-CD3 Monoclonal Antibody (Muromonab-CD3 ) Binds to CD3, a component of T-cell receptor complex involved in antigen recognition cell signaling & proliferation Uses Treatment of acute organ transplant rejection Toxicity “Cytokine release syndrome” High fever, Chills, Headache, Tremor, myalgia, arthralgia, weakness Prevention: Steroids Cytokine release syndrome is a common immediate complication occurring with the use of anti-T cell antibody infusions such as ATG, OKT3 The pathogenesis is that the antibodies bind to the T cell receptor, activating the T cells before they are destroyed. The cytokines released by the activated T cells produce a type of systemic inflammatory response similar to that found in severe infection characterised by hypotension, pyrexia and rigors. the cytokine release syndrome is effectively a type of non-infective fever. Anti-IL-2 Receptor Antibodies (Daclizumab and Basiliximab ) Bind to IL-2 receptor on surface of activated T cells Block IL-2 mediated T-cell activation Uses Prophylaxis of Acute organ rejection Toxicity Anaphylaxis, Opportunistic Infections Anti-TNF Agents TNF – Cytokine at site of inflammation Infliximab Etanercept Adalimumab Infliximab Uses Rheumatoid arthritis Chron’s disease – fistulae Psoriasis Psoriatic arthritis Ankylosing spondylosis Toxicity Infusion reaction – fever, urticaria, hypotension, dyspnoea Opportunistic infections – TB, RTI, UTI Etanercept Fusion protein produced through expression of recombinant DNA. Ligand binding portion of Human TNF-α receptor fused to Fc portion of human IgG1 Uses Rheumatoid arthritis Adalimumab Recombinant human anti-TNF mAb Uses : moderate to severely active crohn’s disease LFA-1 Inhibitor - Efalizumab Monoclonal Ab Targeting Lymphocyte Function Associated Antigen Blocks T-cell Adhesion, Activation, Trafficking Uses Organ transplantation Psoriasis SUMMARY Glucocorticoids – Lympholytic activity, antiinflammatory property. • Used as 1st line immunosuppressive therapy in solid and heamatopoietic stem cell transplant, ITP, RA etc…. • Sirolimus – inhibits protein kinase and inhibits T cell response to IL-2. – Blocks cell cycle progression Thalidomide – inhibits angiogenesis, reduces phagocytosis, enhances cell mediated immunity – Increases levels of IL-10. – Used in multiple myeloma, graft versus host disease, myelodysplastic syndrome, colon and prostrate Cancer. • Mycophenolate Mofetil – mycophenolic acid – Inhibits inosine monophosphate dehydrogenase which is a key enzyme in guanine nucleotide synthesis. – Used in steroid refractory GVHD, RA, SLE. Leflunomide – it inhibits pyrimidine synthesis. Used in RA. • Cyclophosphamide – alkylating agent which destroys proliferating lymphoid cells. Used in SLE, autoimmune haemolytic anaemia, multiple sclerosis, Wegener’s granulomatosis. • Muromonab CD3 – T cell receptor complex ( blocks Ag recognition ). – Used in steroid resistant rejection. • Daclizumab, Basiliximab – IL-2 receptor (blocks IL-2 mediated T cell activation ). – Used in acute organ rejection in renal transplant patients. Azathioprine ( Mercaptopurine ) – interferes with purine nucleic acid metabolism and incorporates false nucleotide. –Used in Renal allograft, RA, SLE, ITP, Crohn’s disease, glomerulonephritis Interferons - IFN alpha- immune enhancing action melanoma. – IFN beta - multiple sclerosis – IFN gamma - chronic granulomatous disease. Immunostimulants Immunostimulants USES: immunodeficiency disorders Chronic infections cancer specific Immunostimulants Levamisole Thalidomide BCG Recombinant Cytokines Interferons Interleukin-2 Other drugs – inosiplex, azimexon, imexon, thymosin, methylinosine monophosphate Immunization Vaccines , Immune Globulin , Rho (D) Immune Globulin Levamisole Antihelminthic Restores depressed immune function of B, T cells, Monocytes, Macrophages USES: Adjuvant therapy with 5FU in colon cancer Used to treat immunodeficiency associated with Hodgkins disease. Toxicity Agranulocytosis Thalidomide Birth defect Contraindicated in women with childbearing potential Enhanced T-cell production of cytokines – IL-2, IFN-γ NK cell-mediated cytotoxicity against tumor cells USE: Multiple myeloma Bacillus Calmette-Guerin Live, attenuated culture of BCG strain of Mycobacterium Bovis It causes activation of macrophages to make them more effective killer cells. used as intravesical therapy for superficial bladder cancer. Adverse Effects Hypersensitivity Shock Chills Interferons Antiviral Immunomodulatory activity Bind to cell surface receptors – initiate intracellular events Enzyme induction Inhibition of cell proliferation Enhancement of immune activities Increased Phagocytosis Interferon alfa-2b Hairy cell leukemia Malignant melanoma Kaposi sarcoma Hepatitis B Adverse reactions Flu-like symptoms – fever, chills, headache CVS- hypotension, Arrhythmia CNS- depression, confusion Interleukin-2 (aldesleukin) Proliferation of cellular immunity – Lymphocytosis, eosinophilia, release of multiple cytokines – TNF, IL-1, IFN-γ Uses Metastatic renal cell carcinoma Melanoma Toxicity Cardiovascular: capillary leak syndrome, Hypotension Capillary leak syndrome (systemic capillary leak syndrome or Clarkson syndrome) A rare medical condition where the number and size of the pores in the capillaries are increased which leads to a leakage of fluid from the blood to the interstitial fluid, resulting in dangerously low blood pressure (hypotension), edema and multiple organ failure due to limited perfusion. Immunization Active – Stimulation with an Antigen Passive – Preformed antibody Active immunization Vaccines Administration of antigen as a whole, killed organism, or a specific protein or peptide constituent of an organism Booster doses Anticancer vaccines: Vaccinating patients with autologous antigen presenting cells (APC) expressing tumorassociated antigens (TAA) Immune Globulin Indications Individual is deficient in antibodies – immunodeficiency Individual is exposed to an agent, inadequate time for active immunization Rabies Hepatitis B Nonspecific immunoglobulins Antibody-deficiency disorders Specific immune globulins High titers of desired antibody Hepatitis B, Rabies, Tetanus Rho (D) Immune Globulin Antibodies against Rh(D) antigen on the surface of RBC prevent the immunological condition known as Rhesus disease (or hemolytic disease of newborn). treating chronic idiopathic thrombocytopenic purpura in Rh-positive patients who have not been splenectomized