The antithrombin-binding structure of heparin
advertisement
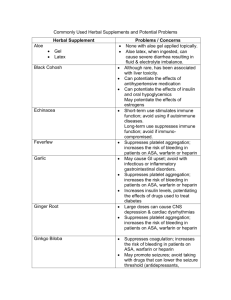
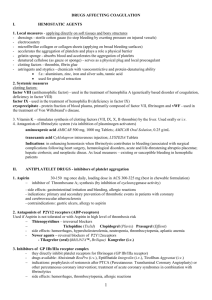
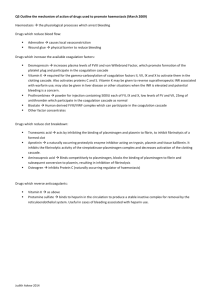
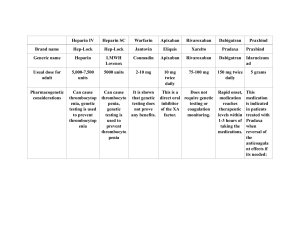
Drugs used in coagulation disorders By S.Bohlooli, Ph.D. Mechanism of blood coagulation Thrombogenesis Blood coagulation Regulation of coagulation and fibrinolysis Fibrin inhibition: 1-antiprotease, 2macroglobulin, 2-antiplasmin, antithrombin Fibrinolysis: plasmin Thrombogenesis Blood coagulation A model of blood coagulation Fibrinolysis Basic pharmacology of the anticoagulant drugs Indirect thrombin inhibitors Direct thrombin inhibitors Warfarin and the Coumarin anticoagulants Indirect thrombin inhibitors Unfractioned heparin Low molecular-weight heparin: Enoxoparin, daltaparin, tinzaprin foundaparinux Differences between fondaparinux, LMWH and HMWH heparin The antithrombin-binding structure of heparin Toxicity Bleeding Thrombocytopenia Caution in patient with allergy Contraindicated in: Hypersensitive Actively bleeding Hemophilia Thrombocytopenia Sever Hypertension Intracranial hemorrhage Advanced renal or hepatic disease Direct thrombin inhibitors Hirudin, lepirudin Bivalirudin Agatroban Melagatran Ximelagatran: oral prodrug Warfarin and the Coumarin anticoagulants Warfarin :Mechanism of action Block the -carboxylation of several glutamate residue in prothrombine and factors VII, IX, and X As well as the endogenous antigoagulant proteins C and S There is 8- to 12-hour delay in the action of warfarin Warfarin :Mechanism of action Warfarin: Toxicity bleeding Readily crosses the placenta Hemorrhagic disorders Abnormal bone formation Cutaneous necrosis Frank infarction of breast, fatty tissues intestine, and extremities Venous thrombosis Basic pharmacology of the Fibrinolytic drugs Contraindications to Thrombolytic Therapy 1. Surgery within 10 days, including organ biopsy, puncture of noncompressible vessels, serious trauma, cardiopulmonary resuscitation 2. Serious gastrointestinal bleeding within 3 months 3. History of hypertension (diastolic pressure >110 mm Hg) 4. Active bleeding or hemorrhagic disorder 5. Previous cerebrovascular accident or active intracranial process 6. Aortic dissection 7. Acute pericarditis Basic pharmacology of Antiplatelet agents Clyclooxygenase inhibitors:Aspirin ADP receptor antagonists: Clopidogrel, ticlopidine Blockers of GP IIB/IIIA receptors: abciximab, eptifibatide, tirofiban Phosphodiesterase inhibitors: dipyridamole, cilostazol Structure of ticlopidine and clopidogrel Toxicity:Ticlopidine nausea, vomiting, and diarrhea severe neutropenia: 2.4% patients Fatal agranulocytosis with thrombopenia Clinical pharmacology of drugs used to prevent clotting Venous thrombosis Risk factors: Anithrombotic management Inherited disorders Acquired diseases Prevention Treatment of established disease Arterial thrombosis Antiplatelet drugs Drugs used in bleeding disorders Vitamin K Plasma fractions Fibrinolytic inhibitors: aminocaproic acid Serine protease inhibitors: aprotinin Vitamin K Vitamin K to promote the biosynthesis of the -carboxyglutamate (Gla) forms of: factors II (prothrombin), VII, IX, and X anticoagulant proteins C and S, protein Z (a cofactor to the inhibitor of Xa) the bone Gla protein osteocalcin, matrix Gla protein, growth arrest-specific protein 6 (Gas6) four transmembrane monospans of unknown function Vitamin K Deficiency increased tendency to bleed Ecchymoses, epistaxis, hematuria, gastrointestinal bleeding, and postoperative hemorrhage fetal warfarin syndrome: vitamin Kdependent protein in bone deficits in bone mineral density and fractures Toxicity Phylloquinone and the menaquinones are nontoxic menadione and its derivatives: hemolytic anemia and kernicterus in neonates, especially in premature infants