572-Sumpradit-_b
advertisement

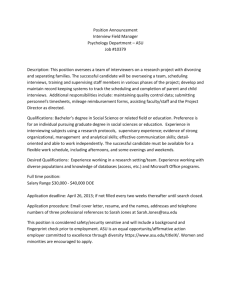
ICIUM 2011 Antalya, Turkey A mixed model to promote rational use of medicines Nithima Sumpradit (1,2); Pisonthi Chongtrakul (3); Kunyada Anuwong (4); Somying Pumtong (4) 1: Food and Drug Administration; 2: International Health Policy Program, Ministry of Public Health; 3: Faculty of Medicine, Chulalongkorn University; 4: Faculty of Pharmacy, SrinakharinwirotUniversity, Thailand On behalf of ASU partners and network ASU partners and network • • • • • • Thai Food and Drug Administration World Health Organization Health Systems Research Institution International Health Policy Program, Thailand National Health Security Office Drug System Monitoring and Development Center • Faculty of Medicine at Chulalongkorn University, Konkean University and Thammasart University • Faculty of Pharmacy at Srinakarintharawiroj University, Chulalongkorn University, Maha Sarakram University • Health professionals and participants from several provinces • Saraburi, Ayutthaya, Samutsongkhram and Ubonratchathani • Kantang community hospital network • Srivichai private hospital network • many other provinces and settings Talk outline • • • • Country’s profile Antibiotics Smart Use Program Lessons learned about policy advocacy Conclusions Country Profile • 63.3 millions population • Universal health care coverage achieved in 2002 • Drug expenditures: 35% of health expenditures. • By law, antibiotics need to be dispensed by a pharmacist. • National Antimicrobial Resistance Surveillance, Thailand (NARST) •National plans and strategies 4 on AMR are being developed. Origin of ASU ASU is an action research to change medicine use behavior. ASU assumptions 1.RUM is behavioral issue. RUM cannot achieve unless it creates behavioral change. 2.Bottom-up approaches are needed to change behavior. Top-down approaches are needed for scaling up and sustain the behavior changed. 5 Objectives To test the ASU model in promoting RUM To reduce unnecessary antibiotic uses in upper respiratory infection (URI), acute diarrhea and simple wound. Individual level - Correct misunderstanding - boost self-efficacy Hospital level - Ensure supportive environment Network level - Decentralized Network National policy level - Link ASU to policy Social level Create a social norm on ASU Predisposing factors Attitudes Subjective norm Self-efficacy Intention Reinforcing factors (by level) e.g., reward and punishment Enabling factors (by level) e.g., Availability of antibiotics, tx guidelines, devices etc Study framework Prescribing behavior Patients’ health & satisfaction Hospital context Community context Phase 1: To test interventions modifying prescribing behavior (2007-8) Setting: 10 district hospitals and 87 health centers in 1 province Phase 2: To test feasibility of scaling up program (2008-9) Setting: 44 hospitals and 627 health centers in 3 provinces (large, medium and small) and 2 hospital networks (public and private) Phase 3: Toward sustainability via policy advocacy, network strengthening and development of new social norms (2010-present) Interventions • Multifaceted interventions (i.e., education, management, incentive and policy/regulation) via decentralized network between central and local partners ASU @ Lumtub community hospital (Krabi province) Buddhist monk as ASU health educator (Saraburi province) Effects on prescribing behavior % of patients who were affected with the targeted diseases and did not receive antibiotics Source: Kunyada Anuwong & Somying Pumtong Effects on patients’ health and satisfaction • Over 80-90% were satisfied with medical services and treatment outcome and intended to return to this healthcare setting for the next medical visit. Source: Kunyada Anuwong & Somying Pumtong Panuchote Tongyoung et al. Effects on scaling up In 2009, National Health Security Office (NHSO), responsible for universal care coverage, announced ASU in an RUM pay-for-performance policy 2007 2008* 2010 •This number does not included the hospitals that adopted ASU prior the policy announcment. Lessons learned about policy advocacy 1. Choosing a right policy Predisposing factors Attitudes Subjective norm Self-efficacy Pay-forperformance criterion (NHSO) Intention Reinforcing factors (by level) e.g., reward and punishment Enabling factors (by level) e.g., Availability of antibiotics, tx guidelines, devices etc Prescribing behavior Patients’ health & satisfaction Hospital context Community context Lessons learned about policy advocacy 2. Multisectoral partners – Authority (Politic, MOH, Government and Healthcare payer) – Academia (University and research unit) – Social movement (NGO and media/social advocator) Modified from a concept of “triangle that moves the mountain” Lessons learned about policy advocacy 3. ‘Proof of success’ Evidence-based policy – Benefits to health – Cost saving – Practical to implement and evaluate 4. Critical mass of ASU alliances & Clear directions – “Climate for change” 5. A window of opportunity Conclusions 1. ASU is an RUM model that can modify antibiotic prescribing behaviors. 2. Scaling up the program requires a policy advocacy via multisectoral partners, decentralized network and evidence-based program. 3. A bottom up approach (at the individual level) is needed to change behavior and a top down approach (and social measures) are needed for scaling up and sustaining the behavior changed.