Class 5 - CatsTCMNotes
advertisement

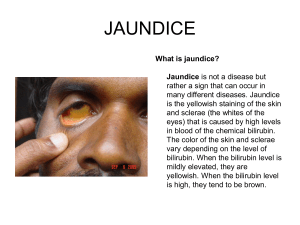
BILIRUBUN METABOLISM AN OVERVIEW 1 FATE OF RED BLOOD CELLS Life span in blood stream is 60-120 days Senescent RBCs are phagocytosed and/or lysed Normally, lysis occurs extravascularly in the reticuloendothelial system (mainly spleen) subsequent to RBC phagocytosis Lysis can also occur intravascularly (in blood stream) 2 NORMAL BILIRUBIN METABOLISM Unconjugated = Fat soluble Conjugated = Water soluble 3 HYPERBILIRUBINEMIA Increased plasma concentrations of bilirubin (> 3 mg/dL) occurs when there is an imbalance between its production and excretion Recognized clinically as jaundice 4 Prehepatic (hemolytic) jaundice Results from excess production of bilirubin (beyond the livers ability to conjugate it) following hemolysis Excess RBC lysis is commonly the result of autoimmune disease; hemolytic disease of the newborn (Rh- or ABOincompatibility); structurally abnormal RBCs (Sickle cell disease); or breakdown of extravasated blood High plasma concentrations of unconjugated* bilirubin (normal concentration ~0.5 mg/dL) *Fat soluble 5 Intrahepatic jaundice Impaired uptake, conjugation, or secretion of bilirubin Reflects a generalized liver (hepatocyte) dysfunction In this case, hyperbilirubinemia is usually accompanied by other abnormalities in biochemical markers of liver function 6 Posthepatic jaundice Caused by an obstruction of the biliary tree Plasma bilirubin is conjugated, and other biliary metabolites, such as bile acids accumulate in the plasma Characterized by pale colored stools (absence of fecal bilirubin or urobilin), and dark urine (increased conjugated bilirubin) In a complete obstruction, urobilin is absent from the urine 7 Diagnoses of Jaundice AST (SGOT)/ ALT (SGPT) = Transaminases ALP = Alkaline Phosphatse 8 Neonatal Jaundice Common, particularly in premature infants Transient (resolves in the first 10 days) Due to immaturity of the liver enzymes High levels of unconjugated bilirubin are toxic to the newborn – cause a type of mental retardation known as kernicterus Jaundice within the first 24 hrs of life or which takes longer then 10 days to esolve is usually pathological and needs to be further investigated 9 Regulation of iron metabolism 10 Overview Patterns of Liver damage Review of individual tests Appraise synthetic function Non-hepatic causes of abnormal tests Synthesize an approach to evaluation 11 What does the Liver do? A LOT! Detoxifies Poisons Stores and Mobilizes Energy Externally-Derived Poisons Controls Blood Sugar (Glucose) Alcohol Regulates Glycogen Byproducts of Metabolism Regulates Fat Storage Bilirubin Aids Digestion Breaks down Drugs Produces Bile Produces Vitamins Regulates Blood Clotting Vitamin D Manufactures Stores Minerals Clotting factors Iron Other Blood Proteins Produces Essential Immune System Produces Hormones Factors Manufactures Cholesterol Monitors, as Well as Manufactures, Countless other Blood Proteins, to Filters Blood Maintain the Proper Levels of Numerous Chemicals in the Body 12 Liver Function Key Points Produces bile Produces proteins Albumin Clotting factors Liver does TOO much for any single test or set of test to determine Focus on the basic test themselves and recognition of basic patterns 13 Markers of Hepatocellular Injury Hepatocytes are damaged so they leak – so these enzymes are HIGH Aspartate aminotransferase (AST/ SGOT) Alanine aminotransferase (ALT/ SGPT) Lactate dehydrogenase (LDH) 14 AST:ALT ratio Alcoholic hepatitis Ratio is >1 90% of the time – often 2:1 Mechanism thought to be related to B6 depletion in alcoholics which leads to disrupted ALT synthesis and therefore decreased levels. This is NOT SPECIFIC!! Viral Hepatitis: Both ALT AND AST elevated Ratio < 1 70% of the time Mechanism unclear 15 Causes of Hepatocellular Damage A Autoimmune hepatitis – ANA, Anti-smooth muscle ab (ASMA), Anti-Liver and Kidney Mitochondrial Ab. HEP A B Hepatitis B C Hepatitis C D Drugs or toxins E Ethanol / Hep E (Pregnancy) F Fatty liver G Growths (i.e., tumors) H Hemodynamic disorder (congestive heart failure or “shock liver”) I Inborn errors - iron (hemochromatosis), copper (Wilson's disease) or alpha1-antitrypsin deficiency 16 Level of Elevation Giannini, E. G. et al. CMAJ 2005;172:367-379 17 Key points AST and ALT elevations infer HEPATOCELLULAR DAMAGE NON-SPECIFIC TEST with other causes that can lead to elevation Levels in the 100’s ETOH, 1000’s viral, and 10,000’s toxin related. Ratio can SUGGEST but not diagnose alcoholic hepatitis 18 Markers of Cholestasis/Obstruction Cholestasis (lack of bile flow) results from the blockage of bile ducts or from a disease that impairs bile formation in the liver itself. Back leads to GRADUAL increase in enzymes over the course of days. Alkaline phosphatase (ALP) Gamma-glutamyltransferase (GGT) Bilirubin 19 ALP Originates primarily in Bone and Liver Other sources include intestine, kidney, placenta. Isoenzymes can determine Bone vs Liver May lag behind symptoms in rising. 20 GGTP (gamma glutamyl transpeptidase): elevated in bile duct disease and alcoholism. 21 Causes of Cholestasis Obstruction Intrahepatic Primary Biliary Cirrhosis – young females. Test: Anti-Mitochondrial Ab (AMA) DRUGS – any number of medications, particularly antibiotics and anti-seizure Any Hepatocellular damage (CONFUSED? The hepatocellular can cause cholestatis, but the necrosis is greater) Critical illness Extrahepatic Common duct obstruction (stone/Tumor) Primary Sclerosing Cholangitis – More often males with IBD Pancreatic head obstruction (Stone/Tumor) Differentiate – use U/S to look at common bile duct dilation. If non-diagnostic do ERCP then liver bx. 22 Bilirubin Fractions Present in Blood and Urine Unconjugated (90%) Conjugated In Serum As: Measured As: Albumin-bound Indirect-reacting bilirubin Unbound Direct-reacting bilirubin Present in Urine Never Yes, when serum bilirubin exceeds 3-4 mg/dL 23 ACUTE ALCOHOLIC HEPATITIS Pattern of liver test abnormality is hepatocellular AST level is higher than the ALT level but rarely exceeds 400 IU/mL AST is typically in the 100 IU/mL to 200 IU/mL range, even in severe disease, and The ALT may even be normal, even in severe cases “In alcoholic hepatitis AST:ALT ratio is 2:1” 24 Jaundice 25 Hyperbilirubinemia Hyperbilirubinemia (Jaundice) Prehepatic (Hemolysis) Hepatic Genetic defects, primary liver disease Unconjugate d Bilirubin Mixed Posthepatic Bile Duct Obstruction Pancreatic Head CA Conjugated Bilirubin 26 Key Points ALP and GGT combined are markers of cholestasis, but other things can make them rise. 2 types of Bilirubin, only conjugated excreted in urine Cholestasis can be extra or intrahepatic – remember how to differentiate 27 LIVER FUNCTION TESTS Protein production Albumin Clotting Factors Total protein production 28 Albumin 65% of serum protein ½ Life = 3 weeks Low levels can correlate with chronic liver dysfunction. Other reasons to be low? Decrease production Malnutrition Chronic Inflammation Increased Loss Kidney – Nephrotic Syndrome GI tract – Protein-losing enteropathy Skin – Severe burn 29 A/G RATIO: The value of the A/G ratio is not precise due to the countless number of variables in the fractions (Total Globulins and Albumin) associated with various metabolic states. Abnormal A/G ratios usually reflect a general index of liver dysfunction. 30 Clotting Factors Most clotting factors are synthesized in the liver ½ shorter than Albumin Prothrombin Time (PT) is a good functional test – but usually use INR to correct for lab variability PT/INR PROLONGED in liver disease 31 Clotting Factor Chronic cholestatic disease often have increased INR– Why? Vit K def Vit K Fat soluable Cholestatic/obustructive so not enough bile secretion so not enough Vit K absorption How to differentiate Vit K def from Decreased synthesis? Give Vit K (take 24-48 hours to correct) Factor V NOT Vit K dependent so can be checked directly 32 Key Points The only liver FUNCTION test are test of PROTEIN PRODUCTION Low albumin due to liver dysfunction implies CHRONIC (>3 week) liver damage Always differentiate Vit K Def from Decreased liver synthesis in pt with cholestatic disease 33 Further Testing Ultrasound Good to visualize large bile ducts and large masses. Cheap. Non-invasive Use: Obstruction ERCP (Endoscopic Retrograde Cholangio Pancreatography) Visualize smaller bile ducts, ampulla of Vater, and head of pancreas. Provides t issue. Expensive. Highly invasive Use: Obstruction Liver Biopsy (rarely done) See hepatic pathology, particularly of the hepatocytes. Gold Standard. Expensive. Invasive Use: Hepatocelluar 34 Overview of Approach to Liver Tests Think of NON-hepatic causes for abnormalities Look at pattern – cholestatic (hepatobiliary) vs hepatocellular Look at tests of FUNCTION for duration of dysfunction What is your DDx? What further testing is needed? 35 Caveats of Liver ‘Function’ Tests There is NO PERFECT TEST A group of tests is needed in order to ‘infer’ functional liver status. Mixed injury/obstruction patterns are common in REAL LIFE !! DO NOT assume that a NORMAL test result indicates absence of liver disease. (example: AST & ALT can be normal in End Stage Cirrhosis.) 36 Hepatitis A Serology 37 Anti-HBsAg HBsAg HBeAg Anti-HBcAg Anti-HBeAg HBV DNA 38 Hepatitis B 39 USA: HCVGenotype distribution 40 Why Genotype? · Genotypes 1, 2 and 3 = North America and Western Europe · Genotype 4 = Africa, Egypt and the Middle East, but is increasingly seen in some parts of Europe ·Genotype 5 = Africa and the Middle East · Genotype 6 = Southeast Asia · Genotype 7 = Central Africa 41 Why Genotype? 1. Those with genotypes 2 and 3: Respond better (require only 24 week therapy) 2. Genotype 1 to respond poorly to therapy with alpha interferon or the combination of alpha interferon and ribavirin. 3. A 48-week course of combination treatment is typically adequate for those with genotype 1. 4. Data are mixed concerning genotype 4, though its response somewhere in between the response of genotypes 2 and 3, and genotype 1. 5. Treating genotype 5 shows that its response to combination treatment is similar to those with genotype 1. 6. genotype 6 lies at an intermediate level, between that seen with genotype 1 and genotypes 2 or 3. 7. Since it has just recently been discovered as having a distinct genetic make-up, the response to standard combination therapy is not yet established for genotype 7. 42 USA: Prev:4 million Incidence:35,000 to 185,000 Deaths: 10,000-20,000 43 Prevalence by Age & Ethnicity USA 44 Hepatitis C 45 VIRAL LOAD TESTS Measures number copies made by a virus Reported as ‘high’ or ‘low’ High: More than 2 million copies Low: Less than 2 million copies ?Log drop: A 10 fold change- take 0ne zero off the end of starting number for each ‘log drop’/’log kill’ 46 RIBA Recombinant Immunoblot Assay The EIA anti-HCV reactivity could represent a false-positive reaction, recovery from hepatitis C, or continued virus infection with levels of virus too low to be detected If the immunoblot test for anti-HCV is positive, the patient has most likely recovered from hepatitis C and has persistent antibody without virus. If the immunoblot test is negative, the EIA result was probably a false positive. 47 PCR (Polymerase Chain Reaction) Amplification PCR amplification can detect low levels of HCV RNA in serum. Testing for HCV RNA is a reliable way of demonstrating that hepatitis C infection is present and is the most specific test for infection. 48 Genotyping and Serotyping of HCV 6 known genotypes and more than 50 subtypes of hepatitis C Helpful in epidemiology and deciding response to therapy Genotypes 2 and 3 are almost three times more likely to respond to therapy with alpha interferon or the combination of alpha interferon and ribavirin. 49 ELISA Enzyme-Linked ImmunoSorbent Assay, or ELISA, is a biochemical technique used mainly in immunology to detect the presence of an antibody or an antigen in a sample. 50 3 ways to test viral loads: PCR measure the amount of HCV RNA in the blood (can measure very small loads as low as 50 IU/mL) bDNA (Branched –chain DNA)- only measures medium loads above 500 IU/mL TMA (Transcription-mediated amplification) can measure very small amounts (5-10 IU/mL) 51 Remember! Antibodies (Ab) suggests immune response IgM-Ab means acute infections IgG-Ab means NO active infection 52 Immunoassay A test that measures the concentration of a substance in a biological liquid: typically serum or urine, uses the reaction of an Antibody (Ab) or antibodies to its antigen (Ag) 53 HBsAg+; X Anti-HBs –ve; Anti HBc Ag +ve; Anti-HBc IGM Ab +ve Suggests: A. B C. D. Acute hepatitis B Chronic hepatitis B-Low infectivity Chronic hepatitis B-High infectivity Immunized against HBV infection 54 HBsAg detected; X Anti-HBs -ve; Anti HBc Ag +ve; X Anti-HBc IGM Ab –ve; Anti- HBe Ab +ve; Suggests: A. B C. D. Acute hepatitis B Chronic hepatitis B-Low infectivity Chronic hepatitis B-High infectivity Immunized against HBV infection 55 X HBsAg not detected; Anti-HBs +ve; X Anti-HBc IGM Ab –ve; Suggests: A. B C. D. Acute hepatitis B Chronic hepatitis B-Low infectivity Chronic hepatitis B-High infectivity Immunized against HBV infection 56 HBsAg detected; X Anti-HBs not detected; X Anti-HBc IGM Ab not detected; X Anti-HBe Ag not detected Suggests: A. Acute hepatitis B B Chronic hepatitis B-Low infectivity C.Chronic hepatitis B-High infectivity D.Immunized against HBV infection 57 HBsAg not detected; Anti-HBs not detected; Anti-HBc IGM Ab not detected; Suggests: A. B C. D. E. Acute hepatitis B Chronic hepatitis B-Low infectivity Chronic hepatitis B-High infectivity Immunized against HBV infection Susceptible to HBV infection 58 PANCREATIC DATA 59 PANCREATIC CANCER ENDOCRINE- INSULINOMA EXOCRINE- HEAD/BODY/ TAIL/AMPULLA OBSTRUCTIVE “PAINLESS” JAUNDICE/ WEIGHT LOSS Fourth leading cause of cancer death DIAGNOSIS BY IMAGING 60 USEFUL BIOCHEMISTRY CMP CA-19-9/ CEA 19 Useful in follow up after therapy but not for diagnosis 61 PANCREATIC DISEASES Endocrine -- which produce the hormones insulin and glucagon Exocrine -- which make powerful enzymes to digest fats, proteins, and carbohydrates 62 PANCREATITIS ALCOHOL T2 DIABETES CYSTIC FIBROSIS PANCREATIC INSUFFICIENCY 63 ? PANCREATIC INSUFFICIENCY Lack of digestive enzymes: presents with symptoms of malabsorption, malnutrition, vitamin deficiencies, weight loss, and is often associated with steatorrhea (loose, fatty, foul-smelling stools). Diabetes may also be present in adults with pancreatic insufficiency. 64 ?Tests Fecal Fat- look for fat globules Trypsin-stool trypsin levels Trypsinogen (serum) Imaging: MRI Studies/ ERCP 65 Pancreatitis Amylase- increase after 2-12 hrs peaks at 12-72 hrs Lipase- increase after 4-8 hrs peaks at 24 hrs Trypsin/Trypsinogen Complete Blood Count (including white blood cell count) Comprehensive Metabolic Panel (Bilirubin, liver function tests) Glucose Calcium Magnesium C-Reactive Protein 66