hepatitis c and tuberculosis
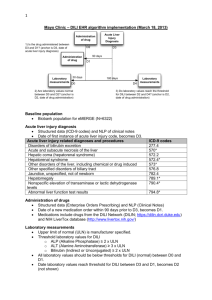
advertisement

hepatitis c and tuberculosis Tumelo Roestoff FCP(SA) Fellow of Gastroenterology Charlotte Maxeke Johannesburg Academic Hospital is there a link between the two entities? Epidemiology >10% 2.5–10% 1–2.5% WHO. Wkly Epidemiol Rec 2002; 77: 41 Impact of hepatitis C infection on TB treatment Definition of DIH (DILI) 1) normal liver chemistry before starting anti-tuberculosis treatment; 1) the patient was receiving INH, RMP or PZA alone or in combination for at least 5 days before the development of abnormal liver chemistry; 2) an increase in ALT and/or AST to ⩾3 times the upper limit of normal (ULN) with symptoms, or an increase in ALT and/or AST to ⩾5 times the ULN without symptoms; 3) no other apparent cause for the elevation of liver chemistry, such as excessive alcohol intake; and 1) removal of the medications re- sulted in a normalisation or at least a 50% improve- ment of the abnormal liver chemistry. “Co-infection with HBV was not associated with a higher rate of hepatitis but was associated with later onset (102 ± 68.7 vs. 37.0 ± 31.9 days, P = 0.01), higher peak alanine amino- transferase level and slower recovery (55.5 ± 62.9 vs. 15.4 ± 10.8 days, P = 0.01).” JY chien et al. Int J tuberc lung disease, 2010; 14(5): 616 - 621 AM J RESPIR CRIT CARE MED 1998;157:1871–1876. • 6 patients relapsed with reintroduction of TB treatment • 2 were excluded because of HIV coinfection • 4 patients consented to interferon alpha 2a therapy – This allowed succesful re-introduction of TB therapy and completion of treatment – Variable response in terms of Hep C viral loads, but no SVR attained in any of the patients UNGO J.R et al, AM J RESPIR CRIT CARE MED 1998;157:1871–1876. Impact of TB on Hepatitis C therapy UPTODATE Pegylated Interferon alpha 2a and Ribavarin Adverse reactions significant ( 1 – 10%) Respiratory: Bronchitis (≥1% to ≤5%), epistaxis (≥1% to ≤5%), nasal congestion (≥1% to ≤5%), nasopharyngitis (≥1% to ≤5%), pharyngolaryngeal pain (≥1% to ≤5%), rhinitis (≥1% to ≤5%), sinus congestion (≥1% to ≤5%), throat sore (≥1% to ≤5%), upper respiratory infection (≥1% to ≤5%), pneumonia (HIV-HCV coinfection: ≥1% to ≤3%) Warnings/Precautions Disease related concerns: Infectious disorders: Interferon therapy may cause or aggravate fatal or life-threatening infectious disorders; discontinue if signs and symptoms occur. Investigate the etiology of any persistent fever during therapy. • Numbers are not overwhelming – controversial as to whether treatment can result in TB infection • Mostly case reports • One study looking at HepC and HIV coinfected population • Adverse effects in treatment Reactivation? Scandinavian journal of infectious diseases; 2006 • 62yr old gentleman • Developed cough and haemoptysis 7months into therapy with Pegylated Interferon and Ribavarin • CT chest suggestive and Montoux was positive, • bronchoscopy and sputum– both smear positive and MTB was cultured • CD4+ depletion to below 290 and abnormal CD4+:CD8+ ratios • Patient was smear positive for a total of 13 weeks on treatment • Subsequent normalisation of CD4+ count with TB treatment J Formos Med Assoc 2009;108(9):746–750] • 55yr old Taiwanese lady • Type 2 Diabetes Mellitus • HepC genotype 2a/2c • Cirrhosis on liver biopsy • Symptoms began 8 weeks in to therapy with combination pegylated interferon alpha 2a and Ribavarin Complication of therapy? - controversial n = 97 TB complicating Hep C therapy in the HIV population Clinical Infectious Diseases 2009;48:e82–5 • Retrospective observational study • 3 hospitals in Madrid Spain • Interferon based therapy for HepC between 1996 and 2007 • HIV and Hep C con-infected patients Results: • 570 patients • 4 developed TB during therapy Key points: • All therapy was discontinued upon diagnosis of TB • Diagnosis was severely delayed – Clinical features were attributed to the side effects of therapy conclusion • Hepatitis C is a risk factor for TB DILI • It appears to be responsible for cases of reactivation of latent TB – May influence clinical practice • It does rarely complicate interferon based HepC therapy in the low incidence areas of the world • ?treatment impact in high TB incidence areas such as Sub-Saharan africa. Thank you