Liver Diseases
advertisement

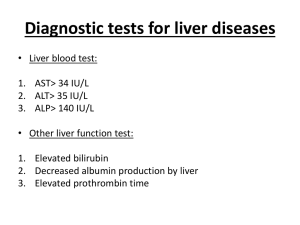
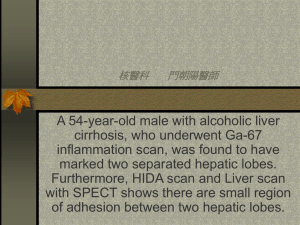
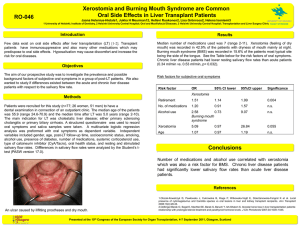
Liver Disease Brenda Beckett, PA-C Liver Large, 4 lobes Highly vascularized – Nutrient-rich blood from GI tract with products of digestion via portal vein – Oxygen-rich blood via hepatic artery Metabolism, detoxification, storage, excretion Ability to regenerate Mechanisms of disease Hepatocyte damage Biliary tract obstruction Metabolic disorders Metallic deposition Fibrotic changes Neoplasms Symptoms of Liver Disease May be asymptomatic until advanced – RUQ abdominal pain – Pruritis – bile salts deposited below skin – Fatigue – Weakness – Decreased libido – Nausea – Bleeding Signs of Liver Disease Gynecomastia Diabetes Testicular atrophy Ataxia / Asterixis Xanthomas, xanthelasmas Jaundice (icterus) Spider angiomata Palmar erythema Hepatosplenomegaly Ascities / anasarca Encephalopathy Fetor hepaticus Caput medusa Asterixis Assessing for Liver Disease Typical patterns in lab tests Many patients with abnormal labs are asymptomatic (need for screening) – Tests for hepatocellular damage – Tests for liver function Hepatocellular Damage Aminotransferases – AST, ALT – Present in hepatocytes. AST also in cardiac muscle. Released with necrosis Alkaline phosphatase – Isoenzymes in liver, bone, gut GGT – Enzyme present in multiple tissues – Nonspecific. Will help to locate liver source Tests for Liver Function Prothrombin time - measures synthesis of factors II and VII Albumin – plasma protein. Maintains oncotic pressure Cholesterol – Not specific, many variables. May be decreased in endstage disease Bilirubin Hemoglobin heme biliverdin unconjugated bilirubin. Combines with albumin to liver. Conjugated and excreted as bile to intestines Elevated in liver disease and hemolysis Jaundice Prehepatic - excess production Hepatic - impaired function (uptake or conjugation) Posthepatic - obstruction Jaundice Unconjugated - (pre and hepatic) Excess production – Hemolytic anemia, hemolysis Hepatic – Causes • Hepatocellular disease, Gilbert’s, neonatal jaundice Jaundice Conjugated (posthepatic) Causes – Obstruction – Hepatocellular disease – Drugs – Sepsis – Post surgical Jaundice Evaluation History – Drugs – prescribed, otc, vit., herbs, etc – Transfusions, IVs, tattoos, IV rec drugs, sexual activity – Recent travel, exposure to jaundiced, alcohol intake – Duration, constitutional symptoms, fever, weight loss, RUQ pain Jaundice Evaluation Physical – Nutrition, signs of chronic liver disease – JV distention, liver and spleen enlargement, – Ascites, tender RUQ Labs – Bilirubin, Conj and Unconj. Liver enzymes Other diagnostic tools Ultrasound Obstruction: – Biliary tract stones – Intrahepatic biliary dilation Texture of liver (fatty vs. cirrhosis) Cystic/solid tumors 17 CT Scan Characterize/quantify lesions Enhancement with contrast Smallest detectable lesion is 1cm Obstruction 18 MRI Best for: – Cystic lesions – Hemangiomas – Iron overload 19 PET Scan Positron emission tomography FDG (Fluorodeoxyglucose) taken up by active tissue and cancer cells Whole body scan Especially to rule out extrahepatic disease in colon cancer patients 20 Percutaneous Biopsy Can be safely done Use US or CT guidance Allows tissue diagnosis 21 22 Alcohol Related Liver Disease Chronic alcohol intake can lead to fatty liver, hepatitis and finally, cirrhosis Fatty liver and hepatitis (inflammation) are reversible, but are precursors to cirrhosis Exact mechanism unknown, but partially due to toxicity and partially due to nutritional deficits Alcohol Related Liver Disease Mechanism not well understood mechanisms – Direct toxicity to hepatocytes – Malnutrition – Immune reactivity after cell damage – Inc risk of Hepatocellular Carcinoma (HCC) Alcohol Induced Hepatotoxicity Alcohol Dehydrogenase primary metabolic pathway – Present in gastric mucosa and liver – Women with less in stomach so more reaches liver Fatty acid & triglyceride deposition 1st response • Fatty Liver or Steatohepatitis in 80%+ EtOH abusers • Usually reversible - may be due to obesity EtOH metabolism products toxic to hepatocytes – Pathologic changes cause hepatitis • • • • Infiltrative PMNs Inflammatory product cell changes Fibrotic changes and cirrhosis Partially reversible Alcohol Related Liver Disease Risk for EtOH disease fxn of quantity and duration of abuse – No correlation to type of beverage – Women develop ARLD with less intake EtOH – 1 beer, 4 oz wine, 1 ounce whiskey has about 12 g of EtOH • Inc risk with intake of >60-80 g EtOH daily for 10 years by men, >20-40 g daily by women Alcohol Abuse Patient may not admit to overconsumption First clue may be liver failure/disease Use transaminase levels for clue, then biopsy to definitively diagnose R/O other causes and comorbidities – HBV, HCV, etc. Cirrhosis Inflammation activates lipocytes – Lose Vit A and form collagen Fibrotic bands form and replace normal cellular architecture Lose compliance firm liver Results in liver function and Portal Hypertension Treatment possible early in process – Treat cause: EtOH, metals, infection, etc. Causes of Cirrhosis Alcohol Viral hepatitis Biliary obstruction Veno-occlusive disease Hemochromatosis Wilson disease Autoimmune Drugs and toxins Metabolic diseases Idiopathic Cirrhosis Manifestations - determined by pathology Scarring and disruption of architecture distorts vascular bed Inadequate blood flow and ongoing damage disturbs hepatocyte function Initially: fatty infiltration Alcohol Related Liver Disease Signs and symptoms: – Often asymptomatic until late. – Hepatomegaly – Anorexia, nausea – Jaundice – Abdominal pain, RUQ tenderness, splenomegaly, ascites, fever, encephalopathy Dx: ARLD Typical blood abnormalities: Incr GGT, AST, ALT (AST>ALT), ALP, Bilirubin. Decr Albumin. Anemia. Prolonged PT Liver biopsy to confirm – Large fatty droplets in fatty liver – Inflammatory changes in hepatitis – Fibrosis with nodular formation, Mallory bodies, destruction of liver architecture in cirrhosis DDX: ARLD US and other imaging to r/o obstruction Hepatitis screening NAFLD can be diagnosed AST/ALT ratio, BMI, MCV and gender Trt: ARLD Abstain from alcohol! Maintain adequate coloric intake Thiamine and folate supplements Cirrhosis: often hospitalization – Low protein diet, monitor lytes, remove ascites, give clotting factors, lactulose to decrease nitrogen absorption from gut Complications of Cirrhosis Chronic Liver Failure Portal hypertension. Causes: – Esophageal varices – Ascites – Encephalopathy Hepatorenal syndrome Hepatopulmonary syndrome Ascites - fluid in abdomen Total body water and sodium excess Cause unknown but 3 theories: – Portal HTN causes sequestration fluid in splanchnic bed dec circulating blood volume – Primary renal process causing retention H2O, Na+ – Portal HTN causes release NO arterial vasodilatation All cause RAA system activation, worsening problem Dec albumin levels dec oncotic pressure to hold fluid in vascular space Ascites Anasarca less common form of same pathophys Inc abdominal girth, weight Dyspnea as fluid restricts diaphragmatic excursion Shifting dullness and US to confirm diagnosis Treat the root cause: fix the liver – – – – Na+ restrict 1500 mg/d Spironolactone initially, add furosemide prn Paracentesis (up to 4-6L) Beware of spontaneous bacterial peritonitis Other Complications Hepatorenal syndrome: cause unknown – Azotemia, hypernatremia, oliguria in presence of histologically normal kidneys • No urinary sediment indicating nephritis – Dx by failure to resolve with hydration – No known treatment Hepatopulmonary syndrome causes hypoxemia – Pulmonary hypertension and R-to-L intrapulmonary shunts – Confused with co-morbid COPD Hepatic Encephalopathy Change in mental status in presence of liver disease – Spectrum from subtle personality changes to confusion to coma EEG changes noted Can cause coma and death Usually follows precipitating event: – GI bleed, sepsis, electrolyte disturbance, shock, sudden inc dietary protein intake Hepatic Encephalopathy Pathophysiology unknown Theory: hepatocellular damage and cirrhosis cause extrahepatic shunting of venous portal blood – Toxic substances not removed from blood Increased serum ammonia level Treat with lactulose up to qid to cause diarrhea (decr nitrogen absorption) Portal Hypertension Classified as: 1) Sinusoidal: Alcoholic cirrhosis 2) Presinusoidal: Splenic/portalvein thrombosis, hepatitis, hepatic fibrosis 3) Postsinusoidal: Vascular outflow problem - Budd-Chiari syndrome: Thrombosis of hepatic veins 41 Portal Hypertension Signs: – Ascites – Caput medusa – Splenomegaly – Variceal bleeding – Encephalopathy Management of Portal HTN 1) 2) Medical: Ascities, encephalopathy, coagulopathy Surgical: TIPS (Transjugular Intrahepatic Portosystemic Shunt), other shunting procedures 43 Acute Liver Failure Acute massive loss of hepatocyte function No pre-existing liver disease or portal HTN Acetaminophen overdose, viral hepatitis, drug toxicity, herbal and dietary supplements 44 Acute Liver Failure Extremely elevated transaminases Bilirubin may be normal Coagulopathies Increased ammonia Acetaminophen overdose: treat with acetylcysteine Acute Liver Failure Can progress to fulminant hepatic failure with encephalopathy – Sepsis – Cerebral edema High mortality rate – May need transplantation No long term sequelae in survivors Uncommon 46 Benign Solid Liver Tumors Hepatic Adenoma - Reproductive age females on OCPs - Sheets of hepatocytes with no parenchymal cells - Risk of rupture and malignant transformation 47 Hepatic Adenoma DX: Difficult to distinguish from FNH (Focal Nodular Hyperplasia) - CT/MRI: to differentiate Can rupture and bleed 48 Hepatic Adenoma Management: <4cm: cessation of OCPs, can regress >4cm, no regression; resection 49 Malignant Tumors of Liver Hepatocellular Carcinoma (HCC) - Associated with cirrhosis, hepB, C - Weight loss, weakness, abdominal pain, hepatomegaly, mass DX: CT scan, perc. biopsy - Will have elevated Alk Phos, AFP 50 HCC Tx: surgical resection - difficult Prognosis: Poor – depends on stage 4-6 months 5 year survival 25% - Death due to cachexia, hepatic failure, mets, bleeding 51 Metastatic Lesions to Liver - Most common neoplasm of liver - Reach liver by portal venous circulation, hepatic artery, direct extension or lymphatic spread - Colon, breast, lung, pancreas, stomach, others 52 Metastatic Lesions DX: CT, labs, PET scan TX: Resection of mets, segments, lobe - Hepatic arterial infusion chemotherapeutic agents - New: Portal vein embolization, radiofrequency ablation 53 Hepatic Resection - Can remove up to 80% - Albumin, synthetic capability by 3rd week - Regeneration by hypertrophy of remaining tissues 54 Wilson Disease Genetic disorder of copper metabolism Impaired biliary excretion of Cu Age 14-30, unless caught in screening Neuro Sx: tremor, ataxia, anxiety, MS Liver: cirrhosis, hepatitis Renal, cardiac involvement Wilson Disease Dx Inc transaminases Dec ceruloplasmin <20 mg/dl Inc urinary copper excretion >100 g/24h Inc liver copper deposition >250 g/g Kayser Fleischer rings Kayser Fleischer rings Wilson Disease Tx Usually lifetime of chelating agents Penicillamine, trientine, zinc Liver transplant for fulminant liver failure Important to catch early Hereditary Hemochromatosis Excess Fe absorption and deposition Caucasians, us. Northern European Early: fatigue, arthralgias, abd pain, impotence Later: diabetes, hepatitis, cirrhosis, cardiomyopathy – Usually age 40-60 depending on comorbidities Screening iron studies HHC Dx Sl. elevated transaminases Incr iron, Transferrin saturation >50% Serum ferritin elev but less specific Genotyping for C282Y and H63D mutations Liver biopsy gold standard but not necessary HHC Tx is Phlebotomy To prevent irreversible end organ damage Phlebotomy 500 cc weekly until mild anemia and ferritin <50 ng/ml May take 2 years initially Maintenance: phlebotomy quarterly Can improve quality of life in patients with liver disease May need transplant Vascular Diseases Acute ischemic injury due to shock, CHF Injury due to chronic congestion from rightsided heart failure – Retrograde elevated venous pressure dilates sinusoids – Poor perfusion results in ischemic injury, loss of metabolic function – Centrilobar fibrosis and cirrhosis – Firm, large liver, other signs liver failure Vascular Diseases Budd-Chiari Syndrome – Occlusion of hepatic veins – Venous thrombosis • Polycythemia Vera, hypercoagulable states, myeloproliferative diseases (cause hypercoagulable state) – Mass or tumor – US or MRI to diagnose – Anticoagulate or TIPS Granulomatous Liver Disease Granuloma: Nodular inflammatory lesion Usually asymptomatic Multiple causes Granulomatous Liver Disease Causes: – Drugs: Allopurinol, quinidine, quinine, etc – Infections: Bacterial, fungal, parasitic, viral – Cirrhosis – Systemic: Hodgkin’s, polymyalgia rheumatica, connective tissue disorders, sarcoidosis Granulomatous Liver Disease DX: – Labs: elevated ALP, GGT – Imaging: US, CT, MRI show calcifications – Biopsy – Often found during imaging for other reasons Granulomatous Liver Disease Treatment: – Treat the cause (stop meds, treat infection, etc) Pyogenic Hepatic Abscess Multiple routes of entry of bacteria – Common bile duct (ascending cholangitis) – Portal vein – Hepatic artery – Direct extension from infection – Trauma Pyogenic Hepatic Abscess Most common bacteria – E. coli – K. Pneumoniae – P. vulgaris – Enterobacter – Multiple anaerobes Pyogenic Hepatic Abscess Signs/Symptoms: – Fever almost always present – RUQ pain – Jaundice Pyogenic Hepatic Abscess Labs: – Leukocytosis, shift to the left – Liver tests nonspecific – Positive blood culture Imaging – CXR: elevated diaphragm on R – US, CT, MRI Pyogenic Hepatic Abscess Treat: – IV antibiotics (3rd gen cephalosporin plus metronidazole. 3-6 weeks – Possible abscess drainage – Treat underlying source