Risk factors for subjective oral symptoms
advertisement
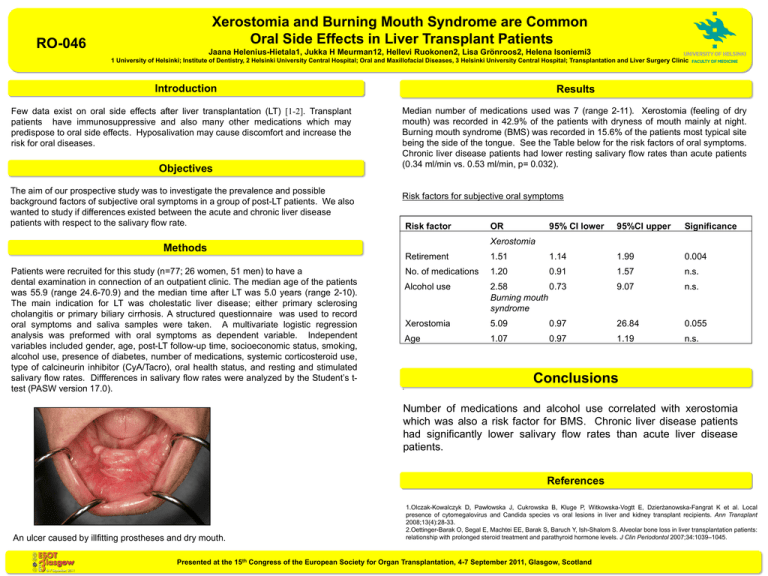
Xerostomia and Burning Mouth Syndrome are Common Oral Side Effects in Liver Transplant Patients RO-046 Jaana Helenius-Hietala1, Jukka H Meurman12, Hellevi Ruokonen2, Lisa Grönroos2, Helena Isoniemi3 1 University of Helsinki; Institute of Dentistry, 2 Helsinki University Central Hospital; Oral and Maxillofacial Diseases, 3 Helsinki University Central Hospital; Transplantation and Liver Surgery Clinic Introduction Few data exist on oral side effects after liver transplantation (LT) [1-2]. Transplant patients have immunosuppressive and also many other medications which may predispose to oral side effects. Hyposalivation may cause discomfort and increase the risk for oral diseases. Objectives The aim of our prospective study was to investigate the prevalence and possible background factors of subjective oral symptoms in a group of post-LT patients. We also wanted to study if differences existed between the acute and chronic liver disease patients with respect to the salivary flow rate. Results Median number of medications used was 7 (range 2-11). Xerostomia (feeling of dry mouth) was recorded in 42.9% of the patients with dryness of mouth mainly at night. Burning mouth syndrome (BMS) was recorded in 15.6% of the patients most typical site being the side of the tongue. See the Table below for the risk factors of oral symptoms. Chronic liver disease patients had lower resting salivary flow rates than acute patients (0.34 ml/min vs. 0.53 ml/min, p= 0.032). Risk factors for subjective oral symptoms Risk factor 95% CI lower 95%CI upper Significance Xerostomia Methods Patients were recruited for this study (n=77; 26 women, 51 men) to have a dental examination in connection of an outpatient clinic. The median age of the patients was 55.9 (range 24.6-70.9) and the median time after LT was 5.0 years (range 2-10). The main indication for LT was cholestatic liver disease; either primary sclerosing cholangitis or primary biliary cirrhosis. A structured questionnaire was used to record oral symptoms and saliva samples were taken. A multivariate logistic regression analysis was preformed with oral symptoms as dependent variable. Independent variables included gender, age, post-LT follow-up time, socioeconomic status, smoking, alcohol use, presence of diabetes, number of medications, systemic corticosteroid use, type of calcineurin inhibitor (CyA/Tacro), oral health status, and resting and stimulated salivary flow rates. Diffferences in salivary flow rates were analyzed by the Student’s ttest (PASW version 17.0). OR . Retirement 1.51 1.14 1.99 0.004 No. of medications 1.20 0.91 1.57 n.s. Alcohol use 2.58 0.73 Burning mouth syndrome 9.07 n.s. Xerostomia 5.09 0.97 26.84 0.055 Age 1.07 0.97 1.19 n.s. Conclusions Number of medications and alcohol use correlated with xerostomia which was also a risk factor for BMS. Chronic liver disease patients had significantly lower salivary flow rates than acute liver disease patients. References An ulcer caused by illfitting prostheses and dry mouth. 1.Olczak-Kowalczyk D, Pawłowska J, Cukrowska B, Kluge P, Witkowska-Vogtt E, Dzierżanowska-Fangrat K et al. Local presence of cytomegalovirus and Candida species vs oral lesions in liver and kidney transplant recipients. Ann Transplant 2008;13(4):28-33. 2.Oettinger-Barak O, Segal E, Machtei EE, Barak S, Baruch Y, Ish-Shalom S. Alveolar bone loss in liver transplantation patients: relationship with prolonged steroid treatment and parathyroid hormone levels. J Clin Periodontol 2007;34:1039–1045. Presented at the 15th Congress of the European Society for Organ Transplantation, 4-7 September 2011, Glasgow, Scotland