Medical Abdomen
Kirstin Blackie
Nima Mohan
Objectives
Be aware of common conditions
presenting with abdominal symptoms
Understand important factors in the
history, examination, investigation and
management of common abdominal
pathologies.
Causes of Abdo Pain
Case Study
Mr C, 35 year old man, presents to his GP with mild
abdominal pain and yellowing of the whites of his
eyes (noticed by his girlfriend who is a nurse).
What other symptoms would you want to ask
about?
Signs and Symptoms of
Liver
pathology
Abdominal pain (RUQ)
Jaundice
Nausea, vomiting Weight loss
Abdo distension
Haematemesis and malaena
Breast swelling, tesicular atrophy
Confusion
Spider naevi
Palmar erythema
Dupuytrens contracture
Hepatomegaly, Spenomegaly
Case study cont:
Has recently has ‘flu’ – has felt
generally unwell, tired and vaguely
nauseated. He is unsure but thinks he
may have had a mild fever.
What risk factors would you ask about?
Risk factors for liver disease
High Alcohol intake
Blood-to-blood contact (IVDU, Tattoos, infected transfusions,
needlestick injuries)
Unprotected sex
Drugs (prescribed, OTC, herbal)
Travel
Family history of liver disease (autoimmune hepatitis, Wilson’s disease)
Mr C is in monogamous sexual relationship with girlfriend for 2
months– she is on OCP. No barrier contraception.
Drinks approximately 30 units alcohol / week. Denies any
other risk factors.
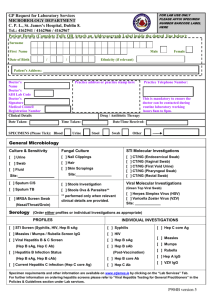
What first line investigations would you like to do?
Liver Function Tests
Viral hepatitis:
Alcoholic hepatitis
ALT greatly raised (10-100x upper limit of normal)
ALT moderately raised (2-10x upper limit of normal)
Drug induced hepatitis
Mixed picture: raised hepatic (AST, ALT) and
Cholestatic (Alk Phos and GGT) markers
Abnormal clotting (prolonged PT or INR) may
indicate acute liver failure
Drugs commonly associated with Hepatitis
Acute hepatocellular damage:
Paracetamol (dose related)
Alcohol (dose related)
TB drugs
Anticonvulsants
Azathioprine
Methotrexate
Chronic active hepatitis
Nitrofurantoin
Isoniazide
Intrahepatic cholestasis
Azathioprine
Oestrogens
erythromycin
Hep A
Hep B
Hep C
Hep D
Hep E
Route of
transmissio
n
Faecal-oral
Blood products,
(contaminate body fluids,
d water/food, sexual contacts
oro-anal
sex)
Blood
products
As for Hep B
Contaminated
water
People at
risk
Childcare
workers,
MSM
vertical
transmission,
sexual partners,
healthcare
workers, Tattoos,
body piercings,
blood
transfusions,
IVDU
IVDU, tattoos
Those at risk
of Hep B or
with chronic
Hep B
Travel to
endemic
areas, and
sporadic
outbreaks
associated
with poor
sanitation eg
refugee
camps
Less
commonly:
vertical
transmission,
sexual
transmission
Potential
for chronic
infection
none
Common in
infants (90%),
rarer in adults
(10%)
80% develop
chronic
infection
Co-infection
with Hep B
none
Incubation
period
3 weeks
(range 2-7)
10 weeks
7 weeks
5 weeks
5 weeks
(range 4-26)
(range 2-21)
(range 3-7)
(range 3-8)
Other causes: EBV, CMV, paravirus B19, dengue, yellow fever.
Hepatitis E endemic areas
Mr C and his girlfriend are both tested for
viral hepatitis
Girlfriend
Mr C
Hepatitis B Serological Markers
65 year old man who hasn’t been to his
GP in years comes into A+E with an
uncomfortable swollen abdomen
What are the differential diagnoses?
5 Fs of distended abdomen
Fat
Faeces
Fluid
Foetus
Flatus
How would you examine for fluid (ascites)?
Shifting Dullness
Does the presence of ascites prove that this patient has liver disease?
What are the possible causes of
ascites?
Cirrhosis: common end point of many
disease processes
Alcohol excess
Hepatitis B
Hepatitis C
Non-alcoholic Fatty Liver disease / Non-alcoholic
Steatohepatitis
Haemachromatosis
Primary Biliary Cirrhosis
Primary Scelosis Cholangitis
Autoimmune hepatitis
Wilson’s disease and other inherited metabolic
disorders
How would you investigate
decompensated liver disease?
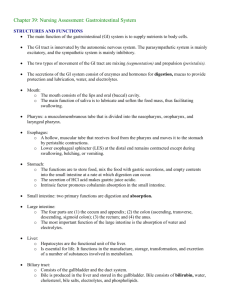
Bloods:
likely increased biliruben, AST, ALT, alk phos, GGT;
Decreased albumin, increased PT/INR (reduced synthetic
function);
Decreased WCC and platelets (hypersplenism);
Look for the cause: serology, autoantibodies, iron studies
Imaging: liver US and doppler, MRI
Ascitic tap:
Biopsy: confirm clinical diagnosis
US liver
“fibrotic,
structurally
abnormal
nodules in liver
…. Compatible
with cirrhosis.
Doppler shows
signs of portal
hypertension.”
Complications of Cirrhosis
Anaemia (folate deficiency, hypersplenism)
Thrombocytopenia (hypersplenism)
Coagulopathy (reduced production of clotting
factors) – can lead to DIC
Oesophageal varices
Spontaneous Bacterial Peritonitis
Hepatic encephalopathy
Hepatocellular carcinoma
How would you manage this patient?
Patient education and support
Treat underlying cause
Adequate nutrition (calorie and protein intake)
Careful prescribing
Therapeutic ascetic tap
Alcohol abstinence (also important in nonalcohol induced cirrhosis)
Monitoring for further complications:
Alcohol dependent individuals will require:
Chlordiazepoxide, Thiamine, Vitamin B
oesophageal varicies or HCC
?transplant
Case Study
“A 17 year old girl presents to the GP with a
8 week history of fatigue. She also reports
frequent episodes of pyrexia and
intermittent episodes of diarrhoea over this
period. Over the last 48 hours she has had
14 episodes of watery diarrhoea”
What other questions would you ask
her???
She denies......
She reports .......
Fatigue – low energy
levels
SOBOE
Palpitations
Frequent Pyrexia
Abdominal pain –
generalised cramps
Diarrhoea – no blood or
mucus
Weight Loss
jaundice, dyspepsia,
vomiting, malena,
constipation, ulcers
Changes in appetite
Changes in mensustral
cycle
urinary symptoms
No recent travel
No changes /
alterations to her diet
What are you going to do
next??
Clinical Examination
Investigations
Urine Dip and MSU
Bloods :
FBC, U&E's , CRP, ESR, LFT's, TFT's, Electrolytes,
Anti -TTG, Blood Cultures??
Stool culture
Imaging
On examination ......
Tachycardic – 101 regular, good
volume.
normotensive – 110/76
WCC
15.9
HB
8.2
MCV
89
Platelets
289
CPT > 3 sec
ESR
HIGH
Pale conjunctive
CRP
110
urea
17
creatnine
110
K+
4.6
na+
135
LFT's
NAD
TFT's
NAD
Cultures
No growth
Cardio- respiratory examination NAD
Diffuse tenderness in the abdomen
normal PR
What is your immediate
management plan?
CROHN'S DISEASE
CLINICAL
FEATURES
EXAMINATION
FEATURES
ULCERATIVE COLITIS
Abdominal pain
Gastro-inestinal bleeding
peri-anal disease
Diahorrea < 6 episodes /day
Constitutuional Symptoms
Rectal Spasm
RIF mass
Scars / Stomas – ileostomy / colostomy bags.
Per-anal skin tags
Fistulas
RADIOLOGICAL
FEATURES
Fistula formation
Rectal involvement
Asymetrical / skip lesions
Superficial ulcers
Rose thorn ulcers
Ileal involvement
ENDOSCOPIC
FEATURES
COMPLICATIONS &
PROGNOSIS
Cobble stone mucosa
Superficial ulceration
Transmural disease
Stud ulcers
Granluoma formation
Pseudopolyps.
Stricture formation
Crypt abscesses
Fistula formation – perianal
Large Bowel obstruction
Toxic megacolon – perforation
Toxic Megacolon
Small bowel obstruction
Primary sclerosing cholangitis.
Malignancy
Increased Risk of Malignancy
WHAT TYPE OF
IMAGING?
NAME OF SIGN?
WHAT DISEASE?
5 OTHER EXTRA
INTESTINAL
MANIFESTATIONS OF
THIS DISEASE?
EXTRA INTESTINAL MANIFESTATIONS
1.
2.
3.
EYES : episcleritis, uveitis
MOUTH: Apthous ulcers,
angular stomatitis
JOINTS : sero-negative
arthropathies (anklysing
spondylitis, sacroilietis)
4.
KIDNEYS : stones fistula,
hydronephrosis
5.
SKIN: Eryhthemna nodosum,
phlebitis, pyoderma
gangrenosum
CROHN'S DISEASE
CLINICAL
FEATURES
EXAMINATION
FEATURES
ULCERATIVE COLITIS
Abdominal pain
Gastro-inestinal bleeding
peri-anal disease
Diahorrea < 6 episodes /day
Constitutuional Symptoms
Rectal Spasm
RIF mass
Scars / Stomas – ileostomy / colostomy bags.
Per-anal skin tags
Fistulas
RADIOLOGICAL
FEATURES
Fistula formation
Rectal involvement
Asymetrical / skip lesions
Superficial ulcers
Rose thorn ulcers
Ileal involvement
ENDOSCOPIC
FEATURES
COMPLICATIONS
&
PROGNOSIS
Cobble stone mucosa
Superficial ulceration
Transmural disease
Stud ulcers
Granluoma formation
Pseudopolyps.
Stricture formation
Crypt abscesses
Fistula formation – perianal
Large Bowel obstruction
Toxic megacolon – perforation
Toxic Megacolon
Small bowel obstruction
Primary sclerosing cholangitis.
Malignancy
Increased Risk of Malignancy
Primary Sclerosing Cholangitis
Strongly association with UC
(less with CD)
Inflammation, fibrosis and
stricture of the intra/ extra hepatic
ducts.
Signs of Live failure
LFTS- Raised Alkaline
Phosphatase, Bilirubin,
hypergamaglobinumina
ANA, ANCA, SMA +VE
Poor prognosis – often need
transplant and increases risk of
cholangiocarcinoma
Management
MEDICAL MANAGEMENT
Treatment of exacerbations :
Mild – oral steroids (Prednislone PO / PR)
Severe – IV Hydrocortisone and Antibiotics
Maintenance therapy :
Maintain adequate nutrition
To prevent exacerbations
5-ASA's (Mesalazine)
Azothioprine
Anti- TNF antibodies
(INFLIXIMAB)
Surgical Management
Surgical management
of complications
Surgical management
of the condition
CASE STUDY
A 25 year old girl presents with a 8 week
history of generalised abdominal cramps
and diarrhoea. They are loose stool, no
blood or mucus and can occur 8-10 times
a day. She also reports that she is
frequently tired and stressed.
What else do you want to know???
Irritable bowel Syndrome
Incidence: common (female 20 -40) ; 40 % people attending
secondary care
6 months of symptoms before diagnosis
Can be predominantly constipation or predominantly diahorrea.
Abdominal pain/ Bloating
Anxiety / depression
Incomplete emptying/ incontinence/ urgency
Constitunal symptoms : tiredness, lethargy, arthalgia, urinary
symptoms, dyspurunina.
RED FLAG SYMPTOMS:
Bleeding, Nocturnal symptoms, weight loss, Age > 50
Treatment Options
Reassurance and support
Address / Treat underlying medical issues
Lifestyle advice :
Dietary modification – excluding food groups.
Smoking and alcohol
Symptomatic relief :
Bloating – Peppermint oil
Constipation – increase fibre and fluid intake
Antispasmodics – mebevrine
Case Study
“A 65 year old man presents with a 4 day history of black
tarry stools. He reports that they are becoming more
frequent and loose. He also reports nausea and one
episode of vomiting this morning.
He also reports that he has a back ache for the past
fortnight and has been taking OTC painkillers for it and
would like you to prescribe some more”
Causes of Upper GI bleeding
Common causes:
Ulcers – Peptic ulcers
(40%)
Varices – Secondary to
portal hypertension (17%)
Gastritis / gastric erosion
Duodenitis
Oesphagitis
Rarer causes:
Mallory -Weiss tears
Angiodysplasia
Bleeding Disorders
Peutz- Jeugher's Syndrome
Osler – Webb – Rendu
Syndrome
Examination / Investigation
On Examination:
He is tachycardic, at 111 bpm / regular and borderline hypotensive
105/72.
He is tender in the epigastrium and peri-umbilically. There is some
voluntary guarding. Bowel sounds are normal.
DRE – Malodorous black tarry stool. No fresh blood.
Investigations:
Bloods : Hb -10.0 , Urea -21 , Creatnine 66, WCC- 7.0, platelets260, CRP – 2.2, LFT's – NAD.
AXR – NAD
Erect CXR – No free air under the diapgram
Management
Bleep : RR -30 BP- 90 /66 , HR -122, CRT > 3, Sats – 94%
A - No airway compromise
B – O2, ABG
C – IV access + Fluid Challenge (which??), Bloods. IV
PPI, erect CXR, AXR
D – GCS, Pupils , Glucose
E - everything else: check notes,
CALL FOR HELP
RE- ASSESS
Rockall Score
Pre-scope score : predicts the morbidity and mortality
Post -scope score : predicts the risk of re-bleeding
Bleeding secondary to ulcers
ABC approach
IV PPI
Endoscopy: CAUTERISTION or CLIPPING of the ulcer
Bleeding secondary to varicies
This is a sign of decompensation
ABC approach
IV Terlipressin (+ \ - Propanalol)
Clotting abnormality – correct it
Octreotide ( often given by seniors)
Secondary prevention (propanolol)
Management of Variceal Bleeding
Sengstaken Blakemore Tube : Balloon Decompression
TIPS : Trans-jugular intrahepatic porto systemic shunt
A catheter into the hepatic vein, guidewire was passed into a portal
vein branch. The tract was dilated with a balloon, and contrast injected.
A metallic stent placed over the wire
TIPS
THANK YOU
ANY QUESTIONS??