wk10 PBL 1 MINUTES - PBL-J-2015

PBL 1: Trigger 1:
Facts
-Vincent M 23
-accompanied by grandmother:
-according to grandmother:
`very tired over the last week
`bit feverish
`lost appetite
-upper abdominal pain
Find out?
-SOCRATES P + associated symptoms of separate symptoms:
`Lethargy?
`appetite?
`abdominal pain?
-detailed history
-define feverish
-medications taken
-down syndrome: more susceptible to any conditions
-mental capacity
Hypothesis
Drug:
-NSAIDS
-Aspirin toxicity
(fever: usually lowers but maybe used in excess)
Infection:
-Viral/bacterial/parasite
-infection H. pylori- Ulcer
-Hepatitis
-Gall bladder stones (inflammation due to obstruction of duct- bile)
-abscess
Metabolic:
-Reflux
-hypothyroidism (downs association)
Tumor/trauma:
-Leukemia (associated with downs)
‘fever, weight loss,
Oxygen:
-bowel ischemia
Psychological:
-panic attack (cause fever)
`anxious
`depression
Findings:
Drugs:
Aspirin(to have serious effects >150mg or 6.5g/24 hours)
NSAIDS(Generally 150-400mg/kg – overdose well tolerated)
Paracetomol (48% poisoning in ER; >4g/24hours but significant effect >7.5-30g/hour)
Microorgamisms:
GIT infections:
Symptoms
`diarrhea, abdominal pain, vomiting, pale bulky stools
Lab tests
‘microscopy, culture, susceptibility
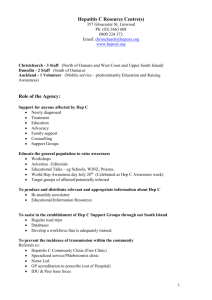
Hepatitis:
Symptoms/signs associated:
Mild fever, malaise, upper abdominal discomfort. Liver inflammation due to virus. Institutionalized intellectually disabled patients at higher risks.
*TRIGGER TWO more likely as *does live institution; dark urine-secondary stage of symptoms; blood transfusion; Jaundice- (dark urine, pale stool)
Leukaemia:
Uncontrolled proliferation of malignant leukocytes
Acute: AML (acute myeloid)
Lowest survival rates (20%)
-abrupt onset
-fever and anemia (from onset) and infections associated
-translocation cr 22 -> Cr 9 (possible downs association)
RISK: haemorrhage/infection
Tumour:
-Renal cancer- renal cell carcinomas (most common)-> associated loss of apetite, abdominal pain.
-hepatic cancer: can have abdominal pain, fever, .. but most likely present with jaundice
-pancreatic cancer can have abdo pain but generally asymptomatic (till late stage) + jaundice
-tumors of diaphragm- often misinterpreted as liver tumors
-stomach,
Depression:
-depression high is downsydrome
-cause abdominal pain-> symptoms: appetite decreased, nausea and constipation
-fever may be caused by antidepressants
Hypothyroidism:
-occurs from an underactive thyroid. Usually has gradual onset cause general symptoms such as constipation, lethargy, weight gain and nausea. Patients particularly at risk include those and down syndrome.
Trigger 2:
Facts Find out? Hypothesis
-only child
-parents separated
-grandmother primary carer
-shared accommodation with other intellectually handicapped people
-moderate degree of intellectual disability
-grandmother
-epilepsy (phenytoin)
-motor vehicle accident: 8 years ago- suffered major abdominal injuries
-required blood transfusions
- recently had nail fold infection: successfully treated with flucloxacillin
-abdominal pain (few days ago)
-Causes of Hepatitis?
-Why dark Urine?
`urine analysis
-Blood transfusion + hepatitis
(other infections)
-phenytoin?
-flucloxacillin?
-stool colour
-vincent says : urine darker than usual no drugs, not sexual active, no IV
Findings:
Dark urine:
-Dark brown but clear -> liver disorder eg. acute viral hepatitis
-Dark yellow/orange -> b-complex vitamins/carotene medications or laxatives
-phenytoin: sodium channel blocker: which prevents hyper excitablity which ceases seizures
PBL 2: Trigger 3
Facts:
-jaundice: sclera and skin
-37.5 degrees Celsius
-enlarged smooth liver
-spleen no palpable
-no ascites
Find out?
-What is Jaundice : mechanisms
-Hep A-E
-Different phases of Hepatitis
Hypothesis
-Hepatitis
-HEP A:
`viral hepatitis (picornavirus)
`transmission faecal-oral (by food handlers, day care, institutions by contaminated food + H20)
`incubation (15-50 days)
`abrupt onset
`symptoms -> abdo pain, jaundice, fatigue
`prognosis -> usually rapid clearance + protective immunity
-HEP B:
`acute hepatitis
`recovery and clearance – most self limiting
`non progressive chronic hep
`fulminant hepitits massive liver necrosis (x)
`asymptomatic c
`incubation 4-26 weeks
*70% DO NOT DEVELOP JAUNDICE
`(Hep D -> life cycle depends on presence of hep B: acute syndrome hard to distinguish from hep B)
-HEP C:
`transmission – blood (x), sexual transmission (x), sharing needles (x)
`incubation- 2-26 weeks
`clinical- (80%) chronic hepatitis-> cirrohosis (x) smooth liver; Hepatocellular(x) ascites
`no vaccine
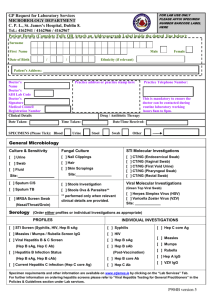
-TESTS:
A: HAV IgM -> recent infection HEP A
IgG ->past infection
B: HbsAg-> active
HB (core) -> recent or past
Antibody to HBsAg – past Hb infection
-or vaccinated
-Hep B type E-> Chronic -> spread?
C: Hep C- detectable
Murtagh’s general practice – UNDER JAUNDICE (good summary of tests)
Trigger 4:
Facts :
-LFT
`ALT 650u/L (0-35)
`AST 450 (0-40)
`APT 186 (35-100)
`GGT 210 (0-250)
`total bilirubin 80 (0-20) glucose normal
-Virology
HBsAG: -ve
Findings
`ALT/AST: hepatocyte breakdown, inflammation
`bilirubin:
`Past Hep B infection as (Anti
HBC : +ve)
`Currently has Hep A infection
(HAV igM: +ve)
‘No Hep C (Anti HCV: -ve)
Hypothesis :
Anti HBV: +ve (all IgG)
Anti HBC: +ve
HBV DNA : -ve
Anti HCV: -ve
HAV IgM : +ve
EBV and CMU: -ve
Trigger 5
Facts:
-grandmother having difficulty with care
-asks if there are any alternatives
Treatment/management
-Tell grandmother it is self limiting; so he needs to rest (6 weeks – 2months0
-Frequent small meals (to allow glucose to be broken down effectively as liver is currently inflamed)
-plenty of fluids
-no alcohol
- phenytoin toxic to liver (monitor dose)
-monitor ALT/AST
Trigger 6
-vaccinations