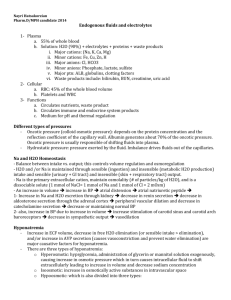
Electrolyte Disorders
advertisement

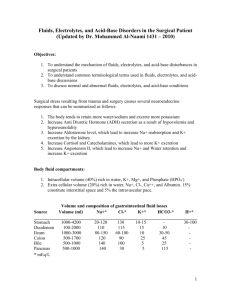
Electrolyte Disorders WS04111: WTD3 Water Metabolism Water intake regulated by: Thirst is the response to water loss ADH release center is close to the thirst center Water loss regulated by: Proximal renal tubular absorption (reabsorbs 125 L/day of the 200 L/ day filtered by glomerulus) Loop of Henle- absorbs sodium and dilutes urine (only sodium is reabsorbed) Collecting duct- controlled by ADH- affects the total amount of urine excreted 2 Sodium Imbalance: Hyponatremia (Low Sodium) (fig.21-1) Hypovolemia:Dehydration/ Diarrhea/Vomiting Renal Salt loss:Diuretics/ ACE inhibitors Hypervolemic:CHF/ Liver disease/ Nephrotic syndrome/ ESRD (ESRD = end stage renal disease) 3 Sodium Imbalance: Hyponatremia Signs and Symptoms Mild ones (130-135) usually asymptomatic (125-130) Nausea and malaise (115-120) Headache/ Lethargy/ Disorientation Red flag: seizure/ coma> cardiac arrest/ death 4 Sodium Imbalance: Hyponatremia- Treatment Replace fluid with iv-0.45% sodium chloride (half normal saline) Asymptomatic casesWater restirction Fludrocortisone 5 Hypernatremia Only when sodium levels are greater than 155clinically significant effects are seen Decreased fluid intake Increased skin loss Increased GI loss (due to loss of water) Renal- ‘osmotic’ diuresis- (hyperglycemia)/ lack of ADH Renal- drugs- lithium 6 Hypernatremia- symptoms and signs Depression, confusion, coma, convulsions Therapy: Free water by mouth IV 5% dextrose Vasopressin/ Thiazides (increase proximal tubular reabsorption of water- reduces water delivery to distal tubule and helps) 7 Sodium Metabolism Primary osmotic agent (mostly ECF) Distal tubule and collecting duct are major regulators of urinary sodium output ?Hormones- Aldosterone (increases sodium reabsorption) controlled by Renin- Angiotensin Atrial natriuretic peptide/ Dopamine/ Prostaglandins- inhibits Na reabsorption CHF-Liver-Nephrotic syndrome-CRF- Steroid- all lead to Na retention Urine sodium excretion less than 20 mEq/L 8 Edema Therapy Restrict dietary sodium (<1 g) Diuretis- loop diuretics- lasix-potassium sparing- aldosterone antagonists (Aldactone) 9 Electrolyte Disorders Potassium Metabolism Potassium Basics Primarily intracellular (3000 mEq) Extracellular (65 mEq) Normal dietary intake 60-90 mEq/day Kidney preserves potassium homeostasis Potassium must be driven into the cellsInsulin/ Epinephrine help the drive Renal- mostly excreted in distal tubule (controlled by aldosterone) More sodium delivered to the tubules more potassium is excreted 11 Hypokalemia (low K) Less than 3.5 mEq/L GI causes: inadequate intake (<10mEq/day) diarrhea/ vomiting (loss of volume= Renin-Angiotensin-Aldosterone-leads to urinaryK loss) K redistribution: Insulin therapy/ Epinephrine/ Folic acid/ B12 therapy/ High bicarb intake/ Periodic paralysis in Asians – thyroid related: defective epinephrine sensitivity 12 Hypokalemia (low K) Renal causes: Diuretics/ Penicillins Adrenal tumors-Aldosteronism/ ectopic ACTH/ Licorice (anise) ingestion- steroid like substance- low K/ HTN/ alkalosis Tobacco chewing- same as above Renin tumors/ Renal artery stenosis CHF Magnesium depletion leads to tubular K wasting 13 Hypokalemia signs and symptoms Neuro-muscular- weakness/ paralysis/ constipation/ ileus/ decreased reflexes/ rhabdomyolysis Cardiac- arrhythmias (if on digoxin+lasix)/ ECGlow amplitude T wave/ depressed ST segment Endoctine- pancreatic insulin release 14 Hypokalemia Therapy Check serum K level Administer potassium chloride- iv / oral 20 mEq oral/day 15 Hyperkalemia Serum K levels greater than 5.5 mEq/L Causes- Rhabdomyolysis/ tissue trauma/ Acidosis/ Renal failure/ Aldosterone deficiency- lead nephropathy, therapy/ Addison’s disease ACEi 16 Hyperkalemia Signs and Symptoms Dangerous! ECG changes happen but not diagnostic (only at high levels more than 6.5 mEq/L) Emergency treatment – Calcium/ Insulin/ beta stimulants/ dialysis/ Resins 17 Electrolyte Disorders Calcium Metabolism Hypocalcemia Most common cause- advanced CRF/CKD (decreased vit D3 and hyperphosphatemia) Magnesium depletion aggravates low calcium symptoms 19 Hypocalcemia Affects muscles and heart Muscle spasms-tetany Laryngospasms/ oral numbness and tingling Chvostek’s sign/ Trousseau’s sign IV Calcium gluconate thrapy Oral calcium and vit D therapy 20 Hypercalcemia More than 12 mg/dL Hyperparathyroidism/ Cancer related Thiazide diuretics Milk-Alkali excess- Tums for calcium use S&S: Constipation/ Vomiting/ Anorexia/ peptic ulcer/ renal stones/ CNS- drowsiness, lethargy, convulsions, Medical emergency coma 21 Electrolyte Disorders Phosphate Metabolism Phosphate Basics Dynamic requirement for cell activity (ATP) Main intracellular buffer Acid-base action (H and P exchange) 85% in bone Dietary intake 1200 mg/day800 mg excreted in urine, 400 in feces PTH regulates P excretion by proximal renal tubule 23 Hypophopshatemia Dietary lack- rare (starvation) Antacid abuse- binds phosphate in the gut Respiratory alkalosis Sepsis- due to impaired WBC chemotaxis Renal: Diabetes/ Excess PTH increases urine phosphate loss Alcoholics- reduced renal threshold 24 Hypophopshatemia-features CNS- coma, convulsions, peripheral neuritis Blood- rare (hemolytic anemia) Muscular- ATP deficits- muscle pain (seen in alcoholics) Bone- increased bone resoprtion Increased urine phosphate levels (more than 100 mg/L) suggests renal causes Treat with oral phosphate 1500-2000 mg/day 25 Hyperphosphatemia Renal failure Acute rhabdomyolysis Tumor lysis Hypoparathyroid 26 Hyperphosphatemia features Hypocalcemia features-low BP ‘Renal osteodystrophy’ Calcification of soft tissues Increased risk of cardiovascular events Therapy- dialysis/ Oral phosphorus binders: calcium carbonate 500 mg thrice daily sevelamer hydrochloride 800-1600 mg daily with meals (adv. No calcium!) Lanthanum carbonate can also be used. thrice 27 Magnesium Basics Second most abundant intracellular cation first) 50% stored in bone, rest in muscles, less 1% in body fluids Acts on myoneural junctions/ cardiac rhythm defects Kidney conserves magnesium Plasma levels 1.5-2.5 mEq/L (K is than 28 Hypomagnesemia Malabsorption Renal- tubular dysfunction Drugs-thiazides/lasix/ antibiotics Hyperaldosteronism 29 Hypomagnesemia- features Muscle twitiching, tremors, weakness Affects renal K reabsorption – leads to hypokalemia Hypocalcemia and hpokalemia may be associated conditions Therapy- oral magnesium- 250-500 mg /day in divided doses 30 Hypermagnesemia Seen in advanced renal disease Iatrogenic-laxatives/antacids Therapy of toxemia of pregnancy Features- muscle weakness, depressed tendon reflexes, ileus, urine retention, low BP Lab- low serum Calcium/ ECG changes Therapy- calcium- antagonist for magnesium 31 Hydrogen ion issues Henderson-Hasselbalch! (Normal HCO3- 24/Pco2-40) pH = 6.1+log HCO3¯ 0.3xPco2 Extracellular pH- 7.4/ Intracellular- 7.0-7.2 Normal metabolism generates- carbonic acid and ‘noncarbonic’ acids- acetoacetate/ ketone (beta-hydroxy butyric acid)/sulfuric and phosphoric acids Carbonic acid mostly exhaled as CO2 Non carbonic acids excreted by kidneys (1 mEq/Kg body wt.) Usually require hospital referral 32