ACS - Clinical Departments
advertisement
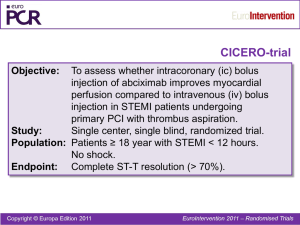
ACS Rogers Kyle, MD 10/2/12 Learning Objectives • Define Acute Coronary Syndrome (ACS) • Review the diagnostic approach to suspected ACS • Review the rationale for risk stratification in ACS • Outline initial management of ACS • Examine antithrombotic options in ACS • Define ACS – UA, NSTEMI, STEMI • Evaluation – Initial evaluation • CP characteristics, EKG, biomarkers Defining ACS • Chest pain - rest, new, increasing – 1/3 none (n/v, syncope, palps, dyspnea) • Old, female, DM • Less intervention, increased mort (JAMA 2000;284 (7):835) • ECG – STEMI • Peaked T (localized inc K+) • J point elev with concave ST • ST elev, convex (no LVH, LBBB) – 2mm in men, 1.5mm women precordial – 1mm in other leads • ST-T merge • OR new LBBB • RV infarct, post-MI • NSTEMI • Down-sloping ST ≥ 0.05 mV in 2 contig leads • And/or T wave inversion ≥ 0.1 mV in 2 contig leads with prominent R or R/S > 1 • Requires biomarker • Non-Diagnostic – 45% (normal in 20%) – Repeat at 20-30 min interval with continued pain Biomarkers • Troponin – Increased sens/spec over CK-MB • Other causes: – Demand ischemia – O2 demand/supply mismatch » Demand – tachy, pre/after load, inc O2 consumption peripherally » Supply – tachy, hypotension, increased filling pressures, hypoxia » Ex - Critical illness, tachy, LVH, vasospasm, CVA/ICH – Direct injury » Defib shock, infiltrative disorders, chemoRx, inflam – CHF » Strain 2/2 vol/pressure overload » Cell death 2/2 neurohumoral stim, cytokines – Pulmonary disease » PE, Pulm HTN – CKD – Burns – Other Management • UA/NSTEMI vs. STEMI • Complex, frequent updates Management ACS • Initial Evaluation – – – – Pain relief Assess hemodynamics – HTN/↓ BP, tachy/brady Estimate risk (TIMI score) Management strategy • STEMI – lytics vs. PCI • UA/NSTEMI – conservative vs. invasive strategy; if invasive, early vs. delayed – Antithrombotics (antiplt and anticoag) – Beta blocker (except when high risk for shock – age > 70, SBP < 120, HR > 110/<60) • IV vs. PO – CCB – Statin, ACE/ARB (AMI, EF < 40%, DM, HTN…?all), aldosterone antag (EF < 40%, CHF) STEMI • • • • Focused update 2009 Pain relief Hemodynamic assessment PCI vs. lytics – Early risk stratification (TIMI score) - ↑ age, ↓ BP, ↑ HR, CHF, AMI – the higher the risk the more beneficial PCI vs. lytics • Antithrombotic/antiplatelet therapy • β-blocker – 2007…2012 update on β-blocker – oral within first 24 hrs if no contraindications; IV only if hypertensive and no contraindications • Statin/ACE/aldosterone antag STEMI Lancet 2003; 361: 13 STEMI • Factors determining reperfusion strategy – Thrombolysis vs. PCI – If early in presentation (< 3 hrs) AND If door to balloon time < 90 min → PCI • > 90 min from PCI → lytics • If PCI related delay < 60 min → PCI; if > 60 min → lytics – “high risk” STEMI → PCI – If between 3-12 hrs → PCI; lytics if PCI related delay ‘significantly greater than’ 120 min – Beyond 12 hrs – no lytics (F XIII) – If no response to lytics → transfer for PCI – If responds to lytics → transfer for PCI ASAP (Transfer-AMI, NEJM; 360:2705-18) TIMI Risk Score STEMI Circulation 2000; 102:2031 TIMI Risk Score STEMI Circulation 2000; 102:2031 STEMI • Factors determining reperfusion strategy – Thrombolysis vs. PCI – If early in presentation (< 3 hrs) AND If door to balloon time < 90 min → PCI • > 90 min from PCI → lytics • If PCI related delay < 60 min → PCI; if > 60 min → lytics – “high risk” STEMI → PCI – If between 3-12 hrs → PCI; lytics if PCI related delay ‘significantly greater than’ 120 min – Beyond 12 hrs – no lytics (F XIII) – If no response to lytics → transfer for PCI – If responds to lytics → transfer for PCI ASAP (Transfer-AMI, NEJM; 360:2705-18) STEMI • Initial therapy – O2, reperfusion strategy – Antiplatelet therapy • ASA 162-325mg (ISIS-2) + P2Y12 (clopidogrel, ticlopidine, prasugrel or ticagrelor) + PPI if GIB risk – Lytics – clopidogrel (others not studied) – For PCI - prasugrel favored over clopidogrel (NEJM 07) – but more bleeds…and ticagrelor too (NEJM 09) • IIb/IIIa inhibitors – depends…on antitcoag (bival vs. hep + IIb/IIIa) and use of P2Y12 (no) and IV vs. intracoronary and agent used (abciximab, eptifibitide, tirofiban); PCI only STEMI – Anticoagulants • PCI (typically d/c’d at end of procedure) – UFH – continue if already begun and add IIb/IIIa or switch to bivalrudin – Lovenox – continue; + IIb/IIIa – Fondaparinux – switch to bivalrudin – Bivalrudin – superior to UFH + IIb/IIIa (HORIZONS-AMI, NEJM 2008; 358:2218-30) • Lytics – UFH, Lovenox, fondaparinux UA/NTEMI • Focused update 2007…and 2011, 2012 • Risk stratification – Immediate high risk – shock, overt CHF, persistent angina, unstable vent. Arrhythmias – Early invasive strategy – 4-48 hrs – TIMI Risk Score (moderate to high risk = score ≥ 3)* Estimate Risk – TIMI Risk Score • Anti-ischemic/analgesic therapy – O2 (Cochrane Review) – Nitrates – SL x 3, then IV if still with pain or htn, chf. (careful with ↑HR, ↓BP, RV infarct, AS/HOCM, viagra) (GISSI-3, ISIS-4); no mortality benefit – MSO4 – relieve pain, anxiety; don’t mask angina – Β-blockers – 40% mortality benefit; no ISA (metoprolol, atenolol); iv or po (avoid with active bronchospasm, brady, pulm edema, ↓BP, ±cocaine) – CCB – if ischemia despite max β –blockade or if contrainicated – Statin – atorvastatin 80mg prior to d/c; LDL < 70 UA/NSTEMI – anti-thrombotic therapy UA/NSTEMI – anti-thrombotic therapy – Antiplatelet therapy • ASA 162 – 325 mg → 75 – 100 mg QD – Clopidogrel if ASA intol • P2Y12 receptor blockers – Add to ASA (CURE. NEJM 2001;345:494) » If conservative strategy – clopidogrel/ticagrelor ± IIb/IIIa (high risk patients) » Invasive strategy (TIMI ≥ 3) • Before PCI – clopidogrel/ticagrelor OR IIb/IIIa (unless on bivalrudin) • At PCI – clopidogrel/prasugrel/ticagrelor OR IIb/IIIa • If initial conservative becomes high risk and goes to angio - clopidogrel/ticagrelor OR IIb/IIIa • if no angio and on ASA/clopidogrel/ticagrelor – can add IIb/IIIa • Prasugrel – – better than clopidogrel if going to PCI (TRITON TIMI-38. NEJM 2007;357:2001). – No worry with omeprazole (not CYP2C19) – Not for pts with prior TIA/CVA, ≥ 75 yrs, < 60 kg – Especially good in DM • Ticagrelor – Better than clopidogrel - PLATO trial (NEJM 2009; 361:1045); + mortality benefit – All ACS, PCI or conservative – Very small excess bleeding – Reversible P2Y12 (vs. clopidogrel, prasugrel) – effects gone in couple of days. – ASA interferes so use < 100 mg/d UA/NSTEMI – anti-thrombotic therapy – Anticoagulation • UFH 60-70 U/kg (5000 max) → 12 U/kg/hr, PTT 50-75 • Enoxaparin – 1 mg/kg Q12 (vs. UFH - may be a little better in conservative strategy)(JAMA 2004; 292:45) • Fondaparinux – 2.5 mg (non-invasive strategy only) • Bivalrudin – 0.1mg/kg → 0.25mg/kg/hr (really only used during cath ≈ UFH + IIb/III) – No lytics in UA/NSTEMI References • Jneid H. et al. (2012) 2012 ACCF/AHA Focused Update of the Guideline for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction. J Am Coll Cardiol 60: 646-681. • Kushner, FG, et al. (2009) 2009 Focused Updates: ACC/AHA Guidelines for the Management of Patients With ST-Elevation Myocardial Infarction. Circulation 120: 2271-2306. • Antman, EM, et al. (2000) The TIMI Risk Score for Unstable Angina/Non-ST Elevation MI JAMA 284 (7): 835-842. • Morrow, DA, et al. (2000) TIMI Risk Score for ST-Elevation Myocardial Infarction. Circulation 102: 2031-2037. • Wiviott, SD, et al. (2007) Prasugrel versus Clopidogrel in Patients with Acute Coronary Syndromes (TRITON–TIMI 38 Investigators) N Engl J Med 357(20): 2001-2015. • Wallentin, L. (2009) Ticagrelor versus Clopidogrel in Patients with Acute Coronary Syndromes. N Engl J Med 361(11): 1045-1057.