Salicylates_TCA Toxicity
advertisement
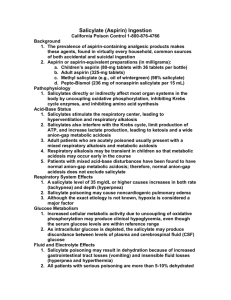
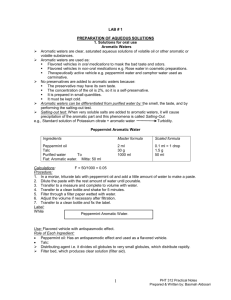
Carson R. Harris, MD, FAAEM, FACEP Regions Hospital Clinical Toxicology Service Emergency Medicine Department Objectives Discuss the toxicological effects of salicylate overdose Identify key management issues Discuss the limitations of the Done nomogram and how to avoid pitfalls of management History and Demographics Hippocrates – 5th century B.C. ▪ Powder from the willow bark 1800s sodium salicylate for arthritis ▪ Abdominal pain Felix Hoffmann ▪ Acetylsalicylic acid (ASA) Introduced 100 years ago ▪ Antipyretic, analgesic, anti-inflammatory History and Demographics Decline in use, but… ▪ Prophylactic for migraine, colon ca ▪ Antiplatelet agent ▪ Decline in incidence of Reye’s Childproof caps – 1970s legislature OTC meds ▪ Combined with antihistamines, caffeine, barbs, and opioids Salicylate formulations Oil of wintergreen: 98% methyl salicylate ▪ 1400 mg/mL Bismuth subsalicylate Aggrenox Therapeutic doses Pediatric 10-20 mg/kg Adults 650-1000 mg q 4-6 hrs ▪ Produce a serum level of 5-10 mg/dL Potential Toxic Acute dose > 150 mg/kg Serious toxicity: 300-500 mg/kg Chronic toxicity: >100 mg/kg/day Peak levels Therapeutic – 1-2 hours Therapeutic EC – 4-6 hours OD – 10-60 hours ▪ Reason for delay ? Concretions, contraction of the pylorus or combination of drugs that delay gastric emptying (opioids and anticholinergics) Liquids absorbed in 1 hr Distribution is facilitated by pH Elimination dependent on dose First order kinetic to zero order ▪ From 4 hours to 15-29 hours A 24-year-old male presented to the ED with nausea, vomiting, tinnitus, and tachypnea after ingesting 100 aspirin tablets. His 4-hour salicylate level was 78 mg/dL; Chem-8 revealed Na 143, Cl 105, K 4.2, HCO3 17; the ABGs showed pH 7.38, pO2 107, and pCO2 27 on room air. He was initially treated with reasonable volume and admitted to the ward. Orders for sodium bicarbonate were given to alkalinize the urine, but this was ineffective in raising urine pH. Approximately 6 hours later the attending was notified that the patient had become confused. He was transferred to the ICU where he was sedated and intubated. Approximately 20 minutes after intubation, the patient rapidly deteriorated and died. ASA is hydrolyzed to salicylic acid Responsible for therapeutic and toxic effects Direct stimulation of respiratory center Medulla Uncouples oxidative phosphorylation Increase in O2 consumption and CO2 production ▪ Increase respiration ▪ Respiratory alkalosis Renal excretion of bicarb, Na and K Metabolic acidosis Inhibition of mitochondrial respiration Increase pyruvate and lactic acid ▪ Metabolic acidosis Disruption of Krebs cycle metabolism and glycolysis Hyperglycemia, ketonemia Dehydration Hyperpnea Diaphoresis Vomiting Fever (increased muscle metabolism) Vasoconstriction of auditory microvasculature Enhance insulin secretion => hypoglycemia Decrease peripheral glucose utilization => hyperglycemia Increase permeability of pulmonary vasculature Increase the production of leukotrienes Stimulate medullary chemoreceptor trigger zone Hematologic effects ASPIRIN Mnemonic Altered mental status (lethargy – coma) Sweating/diaphoresis Pulmonary edema Increased vital signs (HTN, inc RR, inc T, tachycardia) Ringing in the ears Irritable Nausea and vomiting Early Nausea, vomiting, diaphoresis, tinnitus, deafness ▪ Level 25-30 mg/dL Hyperventilation Later Hypotension, NCPE, oliguria, acidemia, cerebral edema, delirium, seizure, coma Classic acid-base disturbance AGMA Respiratory alkalosis with metabolic acidosis Acidemia Increases tissue distribution ▪ Brain, heart, lung Severe hypokalemia NCPE Older patients Smokers Levels >100 mg/dL Acidemia CNS involvement (hallucinations, sz) Chronic toxicity Features Acute Chronic Age Young adult Older adult/infants Etiology Overdose RX misuse Co-ingestions Frequent Rare Mental status Normal Altered Presentation Early Late Mortality Low w/ Rx High Serum levels 40 to >120 30 to >80 Salicylate level Peak 4-6 hr EC and SR preparations late rise Every 2-4 hours until clearly decreasing ▪ Then q 4-6 until <30 mg/dL Always confirm units! ▪ Mg/dL vs. mg/L Done Nomogram (Pediatrics 1960) NOT USEFUL for Chronic ingestions Liquid preparations EC or SR Acidemia Renal failure Unknown time of ingestion Methylsalicylate Severity of ingestion Serum levels Acid-base status Acuteness of ingestion Mental status Bedside Tests Trinder’s reagent – 10% ferric chloride Ames phenistix Chemistry Panel Q 4-6 h LFTs Coagulation studies ABGs APAP Consider: CT, Serum osm, ketones, LP, CO, serum Fe, blood cultures Gastric lavage / WBI Activated charcoal - MDAC Hydration and electrolyte replacement Correct hypokalemia aggressively Urine alkalinization Increase salicylate excretion 1-2 mEq/kg NaHCO3 bolus IV Then 150 mL in 850 ml D5W run 1.5-2 times maintenance Caution in elderly and chronic Monitor UO Dialysis Serum levels > 100 in acute Levels > 60 in chronic Pulmonary edema Renal failure CHF Poor response to standard Rx AMS and acidemia Enteric Coated aspirin Can cause delayed symptom onset Don't wait for clinical deterioration. Alert you nephrology team early and call the poison center even earlier. Serial salicylate levels are imperative. One teaspoon of methyl salicylate contains 7,000 mg of salicylate which is equivalent to approximately 21 regular strength aspirin tablets! The presence of fever is a poor prognostic sign in adults! Cerebrospinal fluid salicylate levels correlate with symptoms better than blood levels The Done nomogram, has limited usefulness Be aware of the proper unit of measure (mg/dL not mg/L or µg/L or mmol/L)! Start potassium supplementation early (in the absence of renal insufficiency) because hypokalemia makes urinary alkalization impossible! Multiple-dose activated charcoal and alkalinization are currently the most popular methods of treatment. Be aggressive. Dialyze early if signs of toxicity are evident. ASA and elderly Impaired renal function ▪ Decreased elimination Impaired hepatic function The risk of salicylate nephrotoxicity is increased with age, Upper gastrointestinal bleed is associated with increased mortality in older age groups. Mortality and Epidemiology From 15% to 1.7% in 1977 Second leading cause of death from overdose in US (Analgesics first). Approximately 500,000 overdoses annually Female, age 20-29, single, employed, no history of drug abuse Approximately 70% die pre-hospital Indications Depression Chronic pain syndromes OCD Panic and Phobic disorders Migraine prophylaxis Peripheral neuropathies Acute Toxic Doses Fatal ingestions range 10-210 mg/kg 2-4 mg/kg is therapeutic, 20 mg/kg is potentially fatal Variable response Absorption Rapidly and completely absorbed Massive OD delays absorption Enterohepatic re-circulation secretes 30% Distribution Wide range in Vd (15-40 L/kg) ▪ Genetic variation ▪ Lipophilic ▪ Elderly has higher Vd Distribution (cont’d) Tissue levels usually 10 times plasma levels Protein binding usually exceeds 90% with some variations ▪ pH dependent Elimination Genetic component Metabolism influenced by other drugs Therapeutic effects Not completely understood Blocks serotonin and NE uptake Anticholinergic effects Cardiac Effects Sinus tachycardia, dysrhythmias ▪ Na channel blockade – quinidine effect Hypotension ▪ Alpha adrenergic blockade and NE depletion Conduction delays / blocks CNS Anticholinergic ▪ Excitation, confusion, hallucination, ataxia Seizures Coma Respiratory Pulmonary edema ARDS Aspiration pneumonia Gastrointestinal Delayed gastric emptying Decreased motility Prolonged transit time Case #1 25 year-old man ingested 60 tablets of Elavil 50 mg each. He presented to the ED about 45 minutes post ingestion agitated and confused. Possibly hallucinating. BP 145/94, P 112, R22, T99.6. He became more agitated and combative and was intubated, lavaged and given AC. EKG revealed QRS 108 with rate 114 What are the critical ECG changes? Prolongation of the QRS complex: ▪ Blockage of fast sodium channels slows phase 0 depolarization of the action potential. ▪ Ventricular depolarization is delayed, leading to a prolonged QRS interval. Patients with QRS intervals >100 ms are at risk for seizures and patient with QRS intervals >160 ms are at risk for arrhythmias. ▪ QRS interval is evaluated best using the limb leads. R wave in aVR >3 mm: ▪ greater selectivity and toxicity to the distal conduction system of the right side of the heart. ▪ effect can be observed as an exaggerated height of the R wave aVR. ▪ may be more predictive of seizure and arrhythmia than prolongation of the QRS complex. R/S ratio >0.7 in aVR QT interval prolongation Arrhythmias How do you treat this? ABCs Activated Charcoal: 30-50 gm Sodium Bicarbonate Dose Endpoint What is the mechanism? Alkalinization appears to uncouple TCA from myocardial sodium channels. Alkalinization may increase protein binding Increases the extracellular sodium concentration improves the gradient across the channel. The initial bolus of 1-2 mEq/kg A constant infusion of sodium bicarbonate commonly accepted clinical practice without any controlled studies validating the optimum administration 100 to 150 mEq of sodium bicarbonate to each liter of 5% dextrose, ▪ the resulting solution is hypotonic or nearly isotonic. What if NaHCO3 doesn’t work? may require treatment with lidocaine and/or magnesium sulfate. Class Ia and Ic agents contraindicated Beta blockers and CCB ▪ Worsen or potentiate hypotension Hypotension, Persistent Direct acting alpha agonists, such as norepinephrine and phenylephrine Dopamine may not be as effective ▪ Require release of endogenous catecholamines that may be depleted during TCA toxicity. Dopamine or dobutamine alone may result in unopposed beta-adrenergic activity due to TCA induced alpha blockade and, therefore, may worsen hypotension. Vasopressin (ADH) What about Seizures from TCA Usually brief (<1 min) self-limiting acidosis increase cardiovascular toxicity. Benzodiazepines Phenytoin is no longer recommended limited efficacy and possible prodysrhythmic. Phenobarbital may be used as a long-acting anticonvulsant. Agitation from TCA Anticholinergic effects Benzodiazepines are also the treatment of choice Physostigmine is contraindicated in TCA overdoses ▪ May cause bradycardia and asystole in the setting of TCA cardiotoxicity. Flumazenil is contraindicated even in the presence of a benzodiazepine co-ingestion. ▪ Several case reports - seizures Emergency department discharge criteria At least 6 hour observation period No significant sign of toxicity during observation period, including normal follow-up ECG prior to discharge Accidental ingestion Appropriate follow-up measures in place Adequately supervised home environment