Acid Base Disorders
advertisement
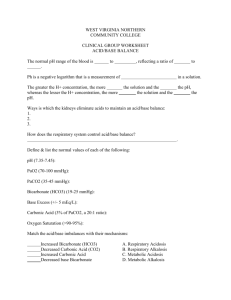
Acid-Base Disorders: Clinical Applications J.B. Handler, M.D. Physician Assistant Program University of New England 1 Abbreviations ABG- arterial blood gas SIADH- syndrome of inappropriate ADH ADH- anti-diuretic hormone Cr- creatinine AVP- arginine vasopressin N- nausea HA- headache OSM- osmolality DI- diabetes insipidus ACEI- angiotensin converting enzyme inhibitor HTN- hypertension HF- heart failure Nl- normal K- potassium Mg- magnesium AMI- acute myocardial infarction S04- sulfate Ca- calcium Nl- normal DKA- diabetic ketoacidosis Resp- respiratory EF- ejection fraction MR- mitral regurgitation DM- diabetes mellitus RRR- regular rate and rhythm 2 Acid-Base Disorders Bicarbonate buffer system CO2 (dissolved) +H2O H2CO3 weak acid H2CO3 H + HCO3 HCO3: weak base; levels regulated by kidneys and maintained for buffering (NaHCO3 is salt) CO2 +H2O H2CO3 H + HCO3 (+ Na) pH=7.40, PCO2= 40mmHg, HCO3= 22-28 meq/L Respiratory center/lungs regulate removal of CO2 Total venous CO2 = dissolved CO2 + (H2CO3) +HCO3 (90-95% of total CO2) Therefore, Total venous CO2 HCO3 3 Acid-Base Disorders Normal metabolism produces 1 meq/L (80 meq/D) of non volatile (H ) acid together with volatile acid (CO2) daily. Body fluid pH is tightly maintained at 7.40 (normal range 7.38-7.42) by continuous removal of H by kidneys and CO2 by lungs. Labs: Arterial pH, PCO2, HCO3 (calculated from arterial blood or measured in venous blood (total CO2.) HCO3 total venous venous CO2 CO2 +H2O H2CO3 H + HCO3 4 Types of Acid-Base Disorders Respiratory and Metabolic Primary respiratory disorders effect PCO2. Primary metabolic disorders effect HCO3. Primary disturbances are accompanied by compensatory changes that move the pH back towards normal but do not fully compensate/correct the primary disorder. Magnitude of compensation depends on how long the disturbance is present. 5 Acid Base Disorders Respiratory Acidosis: pH decreased, PCO2 increased, HCO3 increased (comp.), acute and chronic forms. Respiratory Alkalosis: pH increased, PCO2 decreased, HCO3 decreased (comp.), acute and chronic forms. Metabolic acidosis: pH decreased, HCO3 decreased, PCO2 decreased (comp.). Metabolic alkalosis: pH increased, HCO3 increased, PCO2 increased (comp.). 6 Respiratory Acidosis Primary defect is increased PCO2 as a result of decreased alveolar ventilation. CO2 +H2O H2CO3 H + HCO3 Conditions associated with decreased ventilation: severe COPD; asthmatic who tires; drug OD with suppression of ventilatory drive, neuromuscular diseases. Symptoms: somnolence, confusion (CO2 narcosis), coma, resp. arrest. HCO3 increases (over time), leading to compensation. 7 Expected Changes/Compensation Respiratory acidosis Acute – the pH decreases 0.08 units for every 10mmHg increase in PCO2; HCO3 0.1-1 mEq/liter per 10 mm Hg PCO2 Chronic - HCO3 1.1-3.5 mEq/liter per 10 mmHg PCO2; pH will move towards normal – HCO3 generated by kidneys over days 8 Case 1 Little Billy got into some of dad’s pain meds (hydrocodone). He suffers a significant depression of mental status and respiration. You see him in the ED 3 hours after ingestion with a respiratory rate of 4. A blood gas is obtained. It shows pH = 7.16, PCO2 = 70mmHg, HCO3 = 24 meq/L 9 Case 1 What is the acid/base abnormality? 1. Uncompensated metabolic acidosis 2. Compensated respiratory acidosis 3. Uncompensated respiratory acidosis 4. Compensated metabolic alkalosis 10 Case 1 Uncompensated respiratory acidosis There has not been time for metabolic compensation to occur. As the narcotic toxicity took hold, this child slowed his respirations significantly, PCO2 built up in the blood, and an acidosis ensued. If compensation had occurred the pH would have been higher as a result of an increase in_____? HCO3 11 Treatment of Resp. Acidosis Ventilatory support until the underlying disorder can be corrected. Narcotic antagonists (if applicable) for OD: Naloxone (Narcan) IV-has short half life; may require repeated doses. Benzodiezepine antagonists: Flumazenil given IV may reverse benzodiazepine (OD) induced respiratory depression. Short duration of action. Use with caution. 12 Respiratory Alkalosis Primary defect is decreased PCO2 as a result of increased alveolar ventilation. CO2 +H2O H2CO3 H + HCO3 13 Respiratory Alkalosis Hyperventilation: anxiety, panic attacks, sepsis, CNS insult, cirrhosis, salicylates (overdose), progesterone, mechanical over ventilation, etc. Symptoms- lightheadedness, paresthesias, tetany. Treatment- Address the underlying cause; most cases of anxiety-hyperventilation syndrome are self-limitedrespiratory muscle fatigue. – When acute anxiety is a factor, re-breathing into a paper bag may be useful (short term fix only). 14 Expected Changes/Compensation Respiratory alkalosis Acute – pH increases .08 units for every 10 mmHg decrease in PCO2 ; HCO3 0-2 mEq/liter per 10 mm Hg PCO2 Chronic - HCO3 2.1-5 mEq/liter per 10 mm Hg PCO2 15 Metabolic Acidosis Primary measured defect is decreased HCO3 (combines with increased H ions to buffer) with resultant drop in pH. CO2 +H2O H2CO3 H + HCO3 Compensatory response is decreased PCO2. Excess fixed acids (endogenous) in blood-most common acid-base disorder. Calculation of anion gap is important: Na- (HCO3+CL) 6-12 on newer chem. analyzers which yield higher Cl levels (normal range 98-107 meq/L) than older analyzers. 16 Expected Compensation Metabolic acidosis: PCO2 1-1.5 (mmHg) per 1 mEq/liter HCO3 17 Increase Anion Gap Acidosis pH decreased, HCO3 decreased, Cl normal. Examples: Lactic Acidosis (cardiogenic shock or arrest). Lactate prod. due to inadequate tissue perfusion or hypoxia. DKA-Hyperglycemia with metabolic acidosis; increased production of ß-hydroxybutyric & acetoacetic acids (ketoacidshyperketonemia). Toxins- Ethylene glycol, salicylates, methanol. Uremia (severe renal failure)- endogenous acids. pH < 7.25 common, with HCO3 <16meq/L Anion gap > 12meq 18 Composition of Body Fluids (meq/L) Fluid Na Sweat 30-50 Gastric 40-80 Duodenum 60-120 Bile 145 Pancreas 140 Diarrhea 120-140 Cl 30-50 100 90 100 75 90 K 5 10 5-10 5 5 20 HCO3 0 0 0-10 15-20 115 45 Normal Anion Gap Acidosis (NAGA) Hallmark is acidosis, decreased HCO3 and hyperchloremia. GI HCO3 losses from pancreatic or small bowel contents. – Example: massive (secretory) diarrhea with volume contraction (NaCL and K loss as well); HCO3 secretion in small/large intestine is accompanied by Cl generation/absorption (countertransport); volume contraction leads to NA and Cl retention in the kidney. 20 Renal Tubular Acidosis (NAGA) Hyperchloremic metabolic acidosis without anion gap. Chloride levels are increased. – Distal RTA-deficiency in H secretion by distal nephron; cannot acidify urine; enhanced K secretion (hypokalemia). – Proximal RTA- Inability of proximal tubule to adequately reabsorb filtered HCO3. – Hyporeninemic hypoaldosteronemic RTA: hyperchloremic acidosis with hyperkalemia. Impaired Na reabsorption, K + H secretion. If suspected: nephrology consult 21 Metabolic Acidosis: Sx and Rx Decreased pH leads to hyperventilation, PCO2 resultscompensatory. Additional symptoms reflect underlying disorder. Treatment is specific for the underlying disorder. Example: Diabetic ketoacidosis (DKA) treated with insulin, electrolyte replacement and volume expansion (details in Endocrine module). 22 Case 2 JR has had intermittent vomiting and severe diarrhea for 4 days. He has been unable to keep fluids down and has not urinated in 8 hours. He has a cardiomyopathy with compensated HF. PE: P-90, BP-90/70 with postural changes. He appears lethargic and cool to touch with a prolonged capillary refill time. His arterial blood gas reveals: pH=7.30, PCO2=28mmHg, HCO3=14meq/L. Na-136meq/L, K-3.0meq/L, Cl-110meq/L 23 Case 2 What is the acid/base abnormality? 1. Uncompensated metabolic acidosis 2. Compensated respiratory alkalosis 3. Uncompensated respiratory acidosis 4. Compensated metabolic acidosis 24 Case 2 Compensated metabolic acidosis The prolong history of fluid loss through diarrhea has caused a metabolic acidosis. The mechanisms probably are twofold. First there is lactic acid production from the hypovolemia and tissue hypoperfusion. Second, there may be significant bicarbonate losses in the stool accompanied by generation/absorption of chloride. The body has compensated by “blowing off” the CO2 with increased respirations. 25 Metabolic Alkalosis Hallmark: High HCO3 with increased pH. Most common: Saline responsive metabolic alkalosis, commonly seen with extracellular volume contraction and hypokalemia. Severe vomiting or continuous NG suction: HCl and NaCl losses from stomach initiate the alkalosis and volume contraction. Cl loss (and total body stores) sustains the alkalosis because renal Na reabsorption from volume contraction is accompanied by HCO3 reabsorption (most available anion with Cl depleted). See Case 1 from “Fluid and Electrolyte Disorders” 26 Metabolic Alkalosis Activation of the RAA system to maintain volume results in hypokalemia (Na/K/H exchange in distal tubule) and additional H losses. Hypokalemic, hypochloremic metabolic alkalosis with volume contraction. Entire sequence is rapidly corrected by administering 0.9% saline* (isotonic) with supplemental KCL. The process will self perpetuate until adequate amounts of Na/K/Cl and H2O are available. 27 *AKA- normal saline Expected Compensation Metabolic alkalosis PCO2 0.5-1.0 (mmHg) per 1 mEq/liter HCO3 28 Case 3 A 27 y.o. male is brought to the ED by his girlfriend after being found obtunded at home. PE: P-100, BP-100/60, RR- 6 pH-7.26, PCO2-65mmHg, PO2- 68mmHg, HCO3-31 meq/L What is the primary disorder? Has there been any compensation? What is the correct treatment? 29 Case 4 Following an alcoholic binge, a 54 y.o man presents to the ED with severe N & V x 3 days. He has had only water in the last 36 hrs. PE: P-110, BP- 90/70, 70 syst upright. ETOH on breath, liver enlarged. pH-7.52, PCO2-47mmHg, HCO3-35 meq/L, Na-129 meq/L, K-2.7 meq/L, Cl-84 meq/L. What is the primary disorder? Compensation? Explain the electrolyte abnormalities. What is the treatment plan for this man? 30 Case 5 A 16 y.o with Type 1 DM is brought to the ED after collapsing at home. He is dehydrated, disoriented, hypotensive and his breath has a sweet odor. PE: Ill appearing male c/o abdominal pain. T- 99, P-120, BP- 90/60, RR- 24; skin turgor , mucous membranes dry; lungs- clear; heart- RRR, no murmurs/gallops; abd: soft, non-tender. Urine via catheter- small volume, Sp Gr, ++for glucose and ketones. O2 sat- 97% IV started, fluids running. Labs/ABG: 31 Case 5 (cont.) pH-7.24, PCO2-25 mmHg, HCO3-10meq/L Glucose- 700mg/dl, Na-124 meq/L, K-5.2 meq/L, Cl-98meq/L, Cr-1.0mg/dL, BUN24mg/dL What is the primary disorder? Compensation? What are the sources for abnormal acid production (at least 2)? How do you explain the electrolyte abnormalities? Thoughts on management? 32 Case 6 A 24 y/o med student becomes extremely anxious prior to his board exams. He is brought to the ED with light-headedness, and muscle cramps. P-100, RR-25, BP120/70; remaining exam unremarkable. pH-7.52, PCO2-25mmHg, HCO3-24 meq/L What is the primary acid-base disturbance? Has there been any compensation? What is the treatment for this patient? 33 Case 7 A hospitalized man (medical ward without monitoring) is discovered by the nursing staff unconscious with no pulse or respirations; a “code 99” is called. During the initial response, team members start an IV, and initiate CPR. The initial ABG reveals: pH- 7.01, PCO2- 65mmHg, HCO3- 12 meq/L, PO2- 43mmHg Explain these findings. Management? 34 Case 7 (cont) He is intubated, ventilated and given 100% O2. There is initial delay in getting the defibrillator. CPR is continued. An ABG obtained 3” later reveals: pH- 7.21, PCO2- 41mmHg, HCO3- 13 meq/L, PO2- 280mmHg. Rhythm: V Fib- now ready to defibrillate Explain these findings. Management? 35 Case 7 (continued) Following defibrillation, he stabilizes hemodynamically. He is placed on a ventilator with TV of 900cc, rate of 14; FiO2- .40 ABG 1 hour later: pH- 7.50, PCO2- 26mmHg , HCO3- 22meq/L, PO2- 160 mmHg How do you explain these findings? Management? 36