Pulmonary Hypertension
advertisement
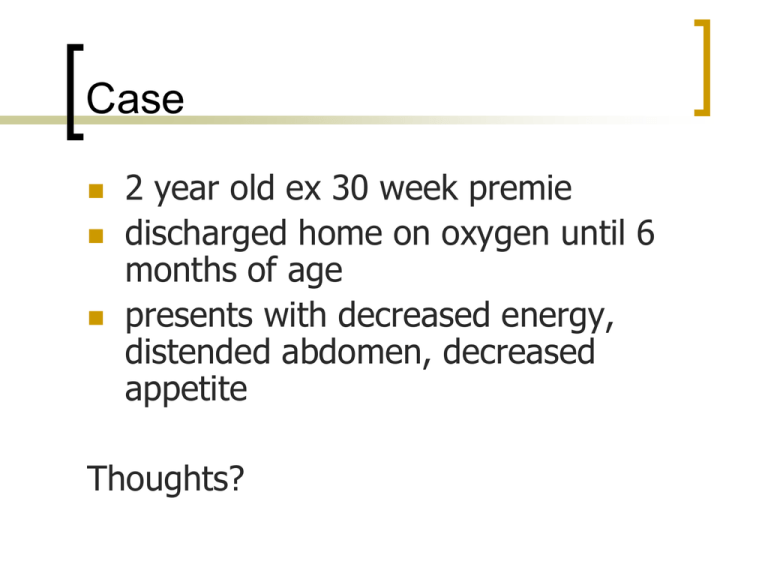
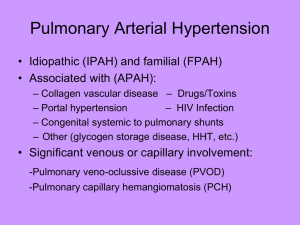
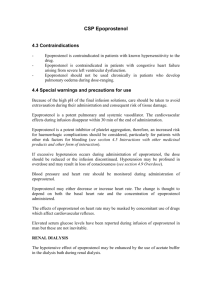
Case 2 year old ex 30 week premie discharged home on oxygen until 6 months of age presents with decreased energy, distended abdomen, decreased appetite Thoughts? Exam PE: no dysmorphic features, PERRL, mmm, some coarse breath sounds but moving air well, RRR with no murmur, right ventricular heave, liver edge 4 cm below RCM, no splenomegaly. Thoughts? Initial Labs Labs: electrolytes and CBCD wnl CXR: mild cardiomegaly with decreased pulmonary markings Initial Labs EKG What study might be helpful next? Echo flat septal wall mild TR with RVPE 55 mmHg above the atrial v wave (systolic BP at time of study = 90) no MR good function Diagnosis? Pulmonary Hypertension The Basics What is it? Normally, pulmonary blood flow occurs in a low pressure, high compliance system High blood pressure in the lungs The walls of the pulmonary arteries constrict The heart has to work harder to pump blood to the lungs “High resistance and low capacity” What defines Vascular Resistance? Ohm’s Law: Voltage (V) = Current (I) x Resistance (R) Pressure (P) = Flow (Q) x Resistance (R) Only at flows > 4x resting flow or pressures > 2x nml does Ohm’s law predict changes in total pulmonary resistance Because of recruitment, PVR decreases with increased pulmonary arterial pressure or flow. Why is it bad? Remodeling of the pulmonary vascular bed Intimal and medial hypertrophy with proliferation of smooth muscle cells and eventual obliteration Pulmonary arteries constrict Right heart must pump against resistance Right heart becomes dilated and less efficient TR Less blood gets out to the lungs and to the body Adaptation to stress, increased activity or growth become impossible Incidence Incidence of PH of various etiologies ~ 2/1000 newborns in the NICU with associated mortality of 10-20%. PH affects 2% of infants following cardiac surgery. Idiopathic PH has a yearly incidence in the range of 1-2/106. History First reported case: 1891 Dr. Romberg in Germany published a description of an autopsy case in which significant thickening of the pulmonary artery was noted in the absence of clearly evident cardiac or lung disease. Formally named: 1951 Dr. Dresdale reported on 39 cases in United States What causes it? 4th World Symposium - 2008 Classification 1. Pulmonary arterial hypertension (WHO group I) a. idiopathic b. familial (10%): AD w/variable penetrance, 2:1 F to M, but M more symptomatic and die younger c. secondary to toxins (fenfluramine (fen-phen), HIV, liver disease (portal HTN), heart disease with shunting to the lungs (PDA, VSD), other diseases (sickle cell, lupus, sarcoidosis) What causes it? 2. Pulmonary venous hypertension (WHO group II) Caused by disease of the left side of the heart (mitral valve disease, pulmonary vein stenosis) 3. PHTN associated with hypoxia and other resp disease (WHO group III) Chronic lung disease, sleep apnea What causes it? 4. PHTN associated with chronic thrombotic disease (WHO group IV) Blood clots in the pulmonary arteries, PE 5. PHTN associated with miscellaneous things (WHO group V) pulmonary capillary disease Heath-Edwards Classification I – Medial hypertrophy II – Intimal hyperplasia III – Occlusive changes (by fibroelastic tissue) IV – Dilation, medial thinning, occlusion V – Plexiform lesions VI – Necrotizing arteritis WHO Classification of Severity Class I: No limitation of usual physical activity; Activity doesn’t cause dyspnea, fatigue, chest pain, or presyncope Class II: Mild limitation of physical activity; no discomfort at rest; but activity causes dyspnea, fatigue, chest pain Class III: Marked limitation of activity; no discomfort at rest but less than normal physical activity causes increased dyspnea, fatigue, chest pain, or presyncope Class IV: Unable to perform physical activity at rest; may have signs of RV failure; symptoms increased by almost any physical activity Pathophysiology Pulmonary vasomotor tone controlled by: Vasoconstrictors Thromboxane ET-1 Leukotrienes Platelet activating factor Vasodilators NO PGI2 Pathogenesis BMPR2 abnormal: vascular hyperplasia and abnormal neovascularization. Three key pathogeneses: • • • Relative decrease in bioavailability of NO Relative increase in serum endothelin-1 Relative deficieny of PGI2/excess of thromboxane A2 platelet dysfxn Intense vasoconstriction: abnormal ATPsensitive K-channels. Immune dysfunction: autoimmune etiology in some cases Diagnosis in Children Dyspnea (60%) Failure to thrive in infancy Fatigue; excessive napping (19%) Diaphoresis Palpitations Syncope Chest pain Occasional hemoptysis All exacerbated by exertion – Doom is impending! Diagnosis – Physical Signs Cyanosis Low output Venous congestion Active right ventricular impulse Loud P2 High frequency TR murmur High frequency diastolic PR murmur Diagnosis - Testing Echo: Purely a screening tool Definitive dx needs direct measure of PAP Identify TR. Add mean RAP to the peak tricuspid jet velocity to get an estimate of peak pulmonary pressure Normal mean PAP at sea level at rest = 12–16 mm Hg PHTN = mean PAP > 25 mmHg at rest and >30 mmHg with exercise Diagnosis requires the presence of above + 2 other conditions: Pulmonary artery occlusion pressure (PAOP or PCWP) < 15 mm Hg Pulmonary vascular resistance (PVR) > 3 Wood units Cath Lab Testing Pulmonary resistance = (PAPmean - LAmean)/ CI expressed as Woods Units and is indexed to BSA Normal < 2, “inoperable” >6 Vasoreactivity testing NO, Flolan, Adenosine—drop in mPAP by 10 mmHg to value < 40 mmHg Predicts CCB response Flolan testing for aortic pressure sensitivity 100% O2 helpful in evaluating lung function Evaluate for septal defects Shed light on the issue of diastolic dysfunction Interpret data in context of patient’s volume status How do you treat it? 1. 2. 3. 4. Improve alveolar oxygenation Minimize pulmonary vasoconstriction Maintain systemic blood pressure and perfusion …No therapy is perfect and none restores normal life expectancy All treatment is palliative. Currently there is no cure Acute Treatments Avoid acidosis and hypercarbia Avoid under or over inflation Avoid preload depletion Avoid inadequate sedation O2 (hypoxia is a potent vasoconstrictor) Hyperventilation (hypocapnia blunts hypoxic vasoconstriction) iNO (FDA approved 12/99). ↑ levels of cGMP in vascular smooth muscle relaxation and inhibition of vascular smooth muscle growth Isoproterenol: beta adrenergic receptor agonistrelaxes airways and increases airflow. pH and PO2 Important for PVR PVR Increases at Lung Volumes Below and Above FRC Lung Volume Goals of Therapy Alleviate symptoms and improve quality of life (exercise tolerance) Improve cardiopulmonary hemodynamics and prevent right heart failure Delay time to clinical worsening Reduce morbidity and mortality “It is not possible to vasodilate vessels that do not exist” The Role of CCBs Primary PHTN Treatment with CCBs in those who respond to acute testing associated with improved 5 yr survival (97% vs 29% non-responding, nontreated patients). (Rich, et al, 1992; Barst, 1999) + responses in 10-25% include decreased PAP & PVR, and increased CI. - responses include increased CHF, decreased CI, and death. Targets for Therapy Humbert et al. New Engl J Med 2004 How do you treat it? Vasoactive medications Prostacyclins Endothelin receptor antagonists Epoprostenol (synthetic prostacyclin (PGI2) aka Flolan®) Treprostinil (Remodulin®), Iloprost (Ilomedin®, Ventavis®) Bosentan (Tracleer®), Sitaxsentan (Thelin®), Ambrisentan (Letairis®) Phosphodiesterase type 5 inhibitors Sildenafil (Revatio®), Tadalafil (Cialis®) RCTs of Approved Agents Class of Drug Study/ Drug N Etiol Class* Design PositiveResults 6 MWD Symptoms Clinical Worsening CPH 6 MWD CPH Symptoms Hepatic toxicity (11%; transient, reversible) Composite Endpoint 6 MWD, sx 6 MWD Symptoms CPH 6 MWD Symptoms CPH Survival Administration 6 to 9 times daily ET-1 Antagonist BREATHE-1 Oral Bosentan/ placebo 213 PAH III,IV DoubleBlind 16-wk PDE-5 Inhibitor SUPER Sildenafil Citrate (20, 40 or 80 mg tid) Doubleblind, placebo 12 wks Prostacyclin analogue Inhalational Iloprost/ Placebo SQ Treprostinil/ SQ placebo 278 IPAH,CT CHD II, III 203 PH III-IV 470 PAH II-IV 81 PPH III,IV Prostacyclin analogue Prostacyclin IV Epoprostenol/ Conventional Rx Doubleblind 12-week Doubleblind 12-wk OpenLabel 12-wk Dis-advantages Headache, flushing, dyspepsia Pain, erythema at infusion site Side effects Indwelling central line Pump (infection,malf) Side effects Phosphodiesterase-5 Inhibitors cGMP Pathway Sildenafil Sildenafil citrate is a selective and potent inhibitor of cGMP-specific phosphodiesterase type 5 (PDE 5) PDE5 is the major subtype in the pulmonary vasculature and is more abundant in the lung than in other tissues Pulmonary vascular cGMP levels can be ↑ by inhibiting phosphodiesterases responsible for cGMP hydrolysis Relatively selective pulmonary vasodilation with little systemic hypotension Recommended for WHO Class II and III Sildenafil In animal models of acute pulmonary hypertension sildenafil decreased pulmonary artery pressures in a dosedependent manner Several case reports now exist suggesting sildenafil is effective Sildenafil Trial Galie, N, et al. Sildenafil Citrate Therapy for PAH. NEJM 2005;353:2148-57. Sildenafil Trial Sildenafil Study in Neonates Sildenafil in neonatal PH due to impaired alveolarisation & plexiform pulmonary arteriopathy M Chaudhari, M Vogel, C Wright, J Smith, S G Haworth Arch Dis Child Fetal Neonatal Ed 2005;90:F527–F528. Sildenafil FDA approved dose is 20 mg tid Higher doses often used given hemodynamic findings Sildenafil – Adverse Effects Abdominal pain, nausea, diarrhea Hypotension, vasodilation, hot flushes Dry mouth, arthralgia, myalgia HA, abnormal dreams, vertigo Dyspnea, abnormal vision, deafness Penile erection, UTI, vaginal hemorrhage Retinitis of prematurity ……… Endothelin Receptor Antagonists Endothelin Clozel. Ann Med. 2003 Endothelin is increased in IPAH and PAH associated with other Diseases Bosentan Specific and competitive antagonist at endothelin receptor types ETA and ETB Blocks the action of ET-1, a neurohormone with potent vasoconstrictor activity in the endothelium and vascular smooth muscle FDA approved 11/2001 Study 351 - Bosentan Channick R, et al. Effects of the dual endothelin-receptor antagonist bosentan in patients with pulmonary hypertension: a randomised placebo-controlled study. Lancet 2001;358:1119-23 BREATHE 1 Trial - Bosentan Rubin LJ, et al. The New England Journal of Medicine; 2002; 346(12):896-903 Walk Distance (meters) BREATHE 1 – 6min Walk Test 60 Placebo (n = 69) Bosentan (n = 144) 40 20 P = 0.0002 Mean ± SEM 0 -20 -40 Baseline Week 4 62.5 mg bid Week 8 125 or 250 mg bid Week 16 BREATHE 1 – Time to Clinical Worsening BREATHE-3 – Bosentan in Kids Inclusion Criteria Age: 2–17 yrs, WHO class II–III PPH or CHD Oxygen sats > 88% Concomitant epoprostenol (Flolan®) (at least 3 months) Exclusion Criteria Liver Disease (ALT/AST > 2 X ULN) Poor Cardiac Fxn (CI < 2 l/min /m2 ) Low BP (Systolic < 80 mm Hg) Dunbar Ivy, UCHS BREATHE-3 - Conclusions Significant hemodynamic improvements were observed after 12 weeks of bosentan Bosentan was well tolerated in children with PAH, either alone or in combination with epoprostenol Bosentan – Who Qualifies? Indication: Treatment of pulmonary arterial hypertension in patients with WHO Class III or IV symptoms, to improve exercise ability and decrease the rate of clinical worsening Bosentan – Lab Monitoring Liver function testing Prior to initiation of treatment and monthly ↑ in ALT, AST or bilirubin. Dosedependent, typically asymptomatic, and reversible after treatment cessation Hemoglobin Prior to initiation of treatment After 1 month, then every 3 months HCG Prior to initiation of treatment and monthly (teratogen) Bosentan – Adverse Effects Cardiovascular: edema (lower limb), flushing, hypotension, palpitations CNS: fatigue, headache Dermatologic: pruritus GI: dyspepsia Hematologic: decrease in H/H Respiratory: nasopharyngitis ~$40,000 per year Prostanoids Prostacyclins Promote vasodilation Inhibit platelet aggregation Inhibit vascular smooth muscle proliferation On treatment algorithm for WHO Class III or IV Only Flolan and Remodulin approved in US Epoprostenol (Flolan ) Actions: relatively locally acting vasodilatation and platelet inhibition Most potent effect -- cardiac output in patients with PAH Resting HR, mean right atrial pressure, and a marked improvement in survival t½ = 3-5 mins Abrupt cessation can be fatal May worsen intrapulmonary shunt initially Contraindicated in veno-occlusive disease Epoprostenol Adverse effects 2˚ delivery system Pump malfunction Catheter related infections Thrombosis Drug-induced side effects Flushing, HA, dizziness, anxiety, hypotension, chest pain N/V, abd pain, diarrhea Myalgias, arthralgias, jaw pain, cramps, dyspnea Thrombocytopenia, rash Tolerance Unstable (Reconstituted daily in alkaline buffer and refrigerated) Cost Outpatient cost up to $100,000 per year (adult) Epoprostenol Epoprostenol Improved exercise capacity and hemodynamics Sitbon, O et al. J Am Cardiol 2002;40:780-88 Epoprostenol/Treprostinil Pump Treprostinil (Remodulin) IV or SQ administration Longer half-life than epoprostenol (4 hrs) Pre-mixed Stable at room temperature BUT Need to change site /pump q3 days Site pain major problem SQ Remodulin 6 minute walk distance compared Simonneau G. et al. Am J Resp Crit Care Med 2002;165:800-804. Iloprost (Ventavis®)Inhalation Solution Indicated for inhalation via the Prodose® AAD® system only 2.5 mcg initial dose increase to 5 mcg if 2.5 mcg dose is tolerated maintain at maximum tolerable dose (2.5 mcg or 5 mcg) 6-9 inhalations daily during waking hours; 8-10 minutes each Properties: Exerts preferential vasodilation in well- ventilated lung regions Longer duration of vasodilation than PGI2 (t ½ = 40 min) Inhalational Iloprost Olschewski et al, NEJM 2002, 347:322-9 Outcomes Some improve Some die rapidly PPHN Lung dx—as the dx improves, so does the PHTN In the absence of a correctable anatomic lesion, reports of spontaneous remission are very rare Pulmonary veno-occlusive disease and CHD leading to cardiovascular collapse within one year Alveolar capillary dysplasia Congenital pulmonary vein stenosis Some get worse slowly Seems to be most common and may need lung transplant Must stay on top of associated OSA, RAD, chronic aspiration and other triggers Who is a Candidate for Lung Tx? PHTN associated with rapid death All previous medical therapy has failed, and the probability of survival for another 2 yrs predicted to be <50%. Nutritional and psychological issues important Time to listing is a function of: Predicted duration of survival Predicted waiting time on transplant list Survival rates: 1 yr = 65-70%, 5 yr = 40-50% Outcome of Children with PHN referred for Lung Tx 8/24 children with PHN referred for LTX died prior to transplant Retrospective application of predictive score (RA x PVR) showed that death prior to tx was predictable (p<0.009) 1/3 of children with PHN are referred for LTX too late to be expected to survive until organs become available. Bridges, et al., 1996 Looking to the Future Better therapies and prevention require a better understanding of the mechanisms which trigger and perpetuate PHN: The genetic basis of the disease The role of proliferation and neovascularization. Better delivery methods for better drugs. Summary Pulmonary arterial hypertension is a progressive disease with significant morbidity and mortality Right heart failure is an important development which clearly prognosticates and marks disease progression Treatment of right heart failure is essential Therapies with proven benefit in transpulmonary hemodynamics, functional class and exercise tolerance include ET-1 receptor antagonism (bosentan), prostanoids, and oral sildenafil. Continuous IV Flolan is reserved for advanced (class IV) disease where there is a proven survival benefit