Neonatal Varicella - Ben Johnson
advertisement

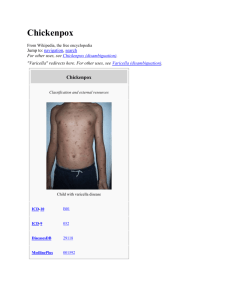
ZS 21 day old ♀ ‘Chicken pox in the neonate’ Content 1. Case presentation 2. Varicella - clinical features - differential diagnosis - treatment - complications - vaccination D1 assessment Call to A&E resus from A&E SpR requesting Paed support S 21/7 old with chicken pox in respiratory distress B 4/7 hx of varicella, with recent infection of sibling. Unremarkable birth history. A Oxygen via NRBM, preparing to obtain iv access and take blds R Immediate attendance of Paeds consultant Assessment in A&E resus A Self maintained, no added sounds. B Self ventilating in air. Sats 92% A. Oxygen applied via NRBM at 10L, sats 100%. Increased effort of breathing. Tachypnoic >70 RR/min. Tracheal tug, recession ++. AE reduced throughout, no wheeze/crackles. C Crt 2-3 sec. Tachycardic 170 bpm. Mild-moderate dehydration. Pale. D BM 4.5. Alert & responsive. Not encephalopathic. Tone, power and reflexes normal. Fontanelle normotensive. Temp 36.8 E Abdomen soft, no organomegally, slightly full. Widespread varicella skin lesions. Immediate management in A&E resus Oxygen to maintain O2 sats >95% iv access Blood cultures, FBC, CRP, U&E, VBG iv cefotaxime & flucloxacillin iv aciclovir CXR Fluid bolus 0.9% normal saline 10ml/kg Maintenance ivf 10% dextrose + 0.18 NaCl Admit Paeds, for incubator care in HDU, continuous sats monitoring VBG in A&E : pH 7.31, pCO2 7.45, pO2 5.64, HCO3 24.2, BE -2.0, Lactate 2.7, Glu 4.5 A&E Resus 020910 2153 PMC 4/7 varicella, 1/7 reduced feeds, 4 hours of respiratory distress. HPC Born AGH 38/40, NVD. Normal preg, scans & birth. ?IUGR in later stages of pregnancy. No SCBU. BW 2.64 kg. Consanguineous parents (1st cousins). Whilst 8 months pregnant, baby’s nephew had chicken pox. Mother therefore given immunoglobulin (see hadn’t had chicken pox before). Baby’s one year old sister has recently had chickenpox which resolved 5/7 ago. Up until this evening, baby has been well. Was feeding by breast 3 hourly, alert, no fever, wet nappies x3/d, BO x2/d HPC Parents have been in touch with GP three times over the phone in the last 5/7. Told “providing feeding well and skin lesions improving then no concerns.” At 1700hrs on day of admission, increased breathing rate and not feeding. Parents phones GP. Told to take to A&E. PMH/ FH Consanguineous parents. Baby’s nephew has a VSD. Had BCG vacc at birth, nil else. Results Blds from A&E CBG After 6 hrs Hb 15.9 WCC 27.3 Neu 14.7 Plt 246 pH 7.32 pO2 5.8 pCO2 7.6 CRP 24 Na 135 K 6.0 Urea 3.0 Cl 95 HCO3- 28.8 BE 1.4 Na 140 K 4.3 Ca 1.02 Cl 102 Glu 4.9 D2 Summary of WR review D2 O2 requirement overnight upto 50%, currently 28% O2 sats 99% RR70, HR 150-200, temp 38.3 despite antipyretic and reduced incubator Temp, ivf 19ml/hr 10% dex + 0.18%NaCl. PU good amounts. BO normal. NBM CBG pH 7.3, pCO2 8.2, HCO3 29.5, BE +1.1, Glu 5.2, Na 139, K4.0 O/E moderate recession, more marked on handling. Resp effort slightly irreg. Tracheal tug & head bobbing. Decreased AE all areas esp RUZ. Widespread fine creps. Crt 3 sec. Irritable on handling. Plan: normal saline bolus 10ml/kg regular CBG NG tube, aspirate air repeat CXR explained to family, may deteriorate further or become tired necessitating respiratory support +/- transfer liase with PICU LGI Wd 17 030910 1047 Day 2 Liaison with PICU consultant LGI: Made aware of possible need for transfer; no further suggestions regarding Mx. PICU team spoke to virologists, nil to add. 1430hrs D2 CBG pH 7.27, pCO2 9.0, pO2 5.8, HCO3 30.3, BE +1.3, Glu 5.5, Na 140, K3.6 Oxygen requirement unchanged. Repeat CXR reviewed, RUZ consolidation improved, still extensive pneumonitis Plan: Needs CPAP May need PICU for ventilation Tolerated nasal CPAP, less tachycardic, improved tachypnoeic, crt <2 sec, O2 100% Consultant reviews on three further occasions with CBG sampling during the afternoon. D2 CBG results day 2 time 0900 1430 1725 2000 2245 pH 7.30 7.27 7.33 7.31 7.36 pCO2 8.2 9.0 7.8 7.38 6.54 4.28 5.24 pO2 5.8 HCO3 29.5 30.3 30.3 27.8 27.6 BE +1.1 +1.3 +2.6 +0.8 +1.6 Na 139 140 141 140 140 K 4.0 3.6 4.8 4.4 4.1 Ca 1.05 1.03 Cl 102 102 4.5 3.5 Glu 5.2 5.5 4.9 CPAP Transferred to PICU D2 Further liaison with PICU consultant LGI throughout the afternoon. Decided that in view of CPAP and possible requirement for ventilation to transfer to LGI. EMBRACE transfer arranged. Arrived at PICU apyrexial and normal obs except RR 55 and O2 94% CPAP. CPAP discontinued as unsettled. Flow-by 5L O2 started. PICU plan : Iv fluids 100 ml/kg/day (0.45% NaCl + 10% dextrose) Start feeds EBM via NGT 2ml/hr and gradually increase if tolerating Continue iv fluclox + aciclovir Switch iv cefotaxime to ceforoxime D/W microbiology mane CBG. Leave off CPAP for time being. Monitor BMs Transferred from PICU day 3 Reviewed mane, no CPAP overnight. Less respiratory distress. O2 96% with flow-by O2 5L. CBG CO2 7.7, pH 7.32. D/W Micro consultant Since ceforoxime has good Step & Staph coverage the fluclox can be Stopped. Ceforoxime is preferred choice over cefotaxime. Recommends send respiratory secretions for viral & bacterial culture. Transferred back to AGH by EMBRACE after only one night at LGI Aciclovir and cefuroxime iv. Ivf and NG feed of EBM at 100ml/kg/day Flow-by O2. Stable D3 Summary of WR review D4 O2 requirement still needing 0.2L/min, afebrile, RR 45-60, HR 140-160 Feeding 3 hourly bolus via NGT, 120ml/kg/day, on aciclovir and ceforoxime. O/E settled, asleep, no resp distress, chest clear, CVS NAD, crt <2 sec, Abdo NAD with 1-2cm liver, healing skin lesions Plan: try breast feeding continue iv meds Summary of WR review D5 Sats 100% on 3L O2. Some short bradycardias overnight. Now on C&G prem. Tolerating some oral feeds. PU’ing. BO. Parents feel she is much better. O/E alert and moving all limbs. Chest clear with some subcostal recession. CVS NAD. ABDO NAD. Fontanelle normotensive. Oral thrush. Clinically nappy rash. Skin lesions heeling well. Plan: start oral nystatin dactarin gel for nappy area continue aciclovir, stop tomorrow on D5 continue iv abx to complete 7/7 course then for oral abx for 7/7 chase blood cultures (NAD) monitor feeding, if struggling then may need to return to NGT feeds Summary of WR review D6 No oxygen requirement overnight. No respiratory distress. Feeding well. Discharged on oral ceforoxime 7/7 48 hr ward access For OPD r/v with Paed consultant in 3/52, repeat CXR OPD 270910 1522 Varicella Chickenpox is a highly infectious, acute contagious disease predominantly of children under 10 years old, though it may occur at any age. Peak incidence Mar – May. It is characterised by fever and a rash, and is caused by varicella zoster virus Around 90% of people who come into contact will develop the disease. Transmission is through 1) direct person to person contact 2) airborne droplet infection 3) through contact with infected articles such as clothing and bedding Around 90% of adults over the age of 18 years have immunity for VZV in the UK Reactivation of latent VZV will result in shingles which is more common in adults In England and Wales, the incidence of chickenpox is approximately 1290 cases per 100,000 person-years gpnotebook.co.uk Varicella – clinical features The incubation period is from 14 up to 21 days chicken pox is infectious from a few days before the onset of rash develops and not more than six days after first lesions appear the rash begins as macular lesions which develop into papular, or vesicular lesions (filled with fluid) and later becomes pustular chickenpox rash has a centripetal distribution - mostly on the face and trunk and sparsely on the limbs there is erythema around the lesions and they are intensely itchy usually the rash peaks at around 48 hours in immunocompetent people vesicles dry and crust over, and sometimes scar if scratched to excess oropharynx and genital tract mucous membranes may be involved as well new lesions can emerge for up to 5 days gpnotebook.co.uk Varicella In children under 10 years, the disease is usually mild and self limiting, but a more severe infection can be seen in 1) adults - especially in pregnant women and in smokers since they are at an increased risk of developing fulminanting varicella pneumonia 2) neonates 3) immunosupressed individuals – there is an increased risk of developing disseminated or haemorrhagic varicella Signs of severe infections include: •respiratory symptoms (clinical respiratory signs are often absent). •densely cropping vesicles •haemorrhagic rash •bleeding from gums, haemoptysis, GI bleeding •any neurological changes - cerebellar signs, encephalopathy •persisting fever with new vesicles >6 days after onset General recommendationis for school exclusion for 5 days from onset of rash gpnotebook.co.uk Differential diagnosis • • • • • • • • • • herpes simplex disseminated herpes zoster impetigo drug related eruptions contact dermatitis erythema multiforme Stevens Johnson syndrome hand, foot and mouth disease scabies disseminated molluscum contagiosum gpnotebook.co.uk Treatment Treatment is usually symptomatic in milder disease paracetamol or ibuprofen can be given to reduce flu like symptoms, fever and pain antivirals should be considered for patients who presents within 24-48 hours of new vesicles (indicating an evolving disease) antiviral therapy should be continued for at least 1 week oral aciclovir may also be given to 1) immuocompetent adults and older adolescents 2) Infants 3) severe infection at any age 4) immunosuppression 5)severe cardiorespiratory disease 6) chronic skin disorder Varicella zoster immune globulin (VZIG) VZIG prophylaxis can be used in individuals who complete all of the following criteria: •significant exposure to chickenpox or herpes zoster •a clinical condition that increases the risk of severe varicella, this includes immunosuppressed patients, neonates and pregnant women •no antibodies to VZ virus Immunosuppressed patients should be given immunoglobulin to varicella zoster and aciclovir within two days of contact with varicella. If they develop chicken pox they should be treated with aciclovir. Antibiotics should be given for secondary infections gpnotebook.co.uk Complications Majority of children recover without any complications but neonates, adults, pregnant women and those who are immunocompromised may have more serious complications Pulmonary involvement…….5-14% of adults CNS involvement…….cerebellar ataxia and/or encephalitis Secondary bacterial infections….inc osteomyelitis Haemorrhagic complications…..GI bleeds, DIC, cerebral bleeds In pregnancy…..significant maternal mortality and congenital VAR syndrome Others….. arthritis, glomerulonephritis, myocarditis, and purpura fulminans gpnotebook.co.uk Varicella vaccination Varicella vaccine is a lyophilised preparation which contains live attenuated organisms of the Oka strain of varicella zoster virus. •should be administered as deep subcutaneous injection and can be given together with other live vaccines such as MMR •children from one year to under 13 years of age; a single dose of varicella vaccine will give protection for around 90% of children •children aged 13 years or older and adults - should receive two doses of varicella vaccine four to eight weeks apart, around 75% will have protection against clinical chickenpox (1) gpnotebook.co.uk