presentation
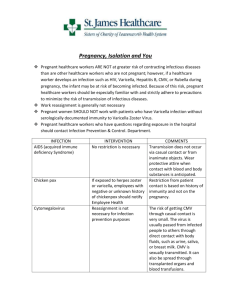
advertisement

Immunisations and Infections Helen Toyne, GP Toby Angstmann, O&G Ashley Watson, Infectious Diseases Case 1: Mrs A: Planning her first pregnancy • • • • 29 years of age Never been pregnant Works as primary school teacher Thinks she had childhood immunisations, no physical record • No known history of varicella infection • Several tattoos acquired in Bali 5 years previously Case 1 Mrs A: Routine care, individualised care • Syphillis, Rubella, Hep B Antigen, HIV, varicella IgG, UMCS • Other possibilities: – – – – – Hep B sAntibody (if immune, no more tests!) Hep C chlamydia Parvovirus B19 ?? Not routinely screened Measles antibody – may be relevant in some people, outbreak at present – Bacterial vaginosis HVS – not antenatal, not first preg. Parvovirus B19: • Also known as fifth disease, slapped cheek syndrome, erythema infectiousum • 50% women immune pre-pregnancy • If infected during pregnancy, less than 5% have miscarriage/anaemia • Serology availability and indications? • When/ if to stay away from work (kids infectious 48 hours before symptoms) Toby’s video here • Severe consequences possible • 4 cases TCH past 12 months Pre-pregnancy immunisations • • • • Influenza MMR (live virus) DTPa Varicella (live virus) • What about early pregnancy – fever?? Whooping cough outbreak from 2009 Influenza in the ACT – per CHO • Influenza in neonates: ACT Data • In 2012, there were 17 cases of influenza in infants aged 12 months or less. • Of those, 6 were aged 3 months or less, one was aged 4 weeks National FluCan data – pregnant women • Between 4 April to 12 October 2012, – 39 pregnant women hospitalised with influenza, accounting for – 3.5% of all hospitalisations due to influenza. – 2 were in ICU. Case 2 - Antenatal • Mrs H, 26 weeks pregnant, 2nd baby • Immunised 3 year old son has mild varicella illness • She does not recall having chicken pox or immunisation – Which test – How to get ZIG • What if child 18months with vaccine associated varicella? Case 3 - Antenatal • Mrs C, 36 weeks pregnant • Copious white vaginal discharge, perineal itch • History of recurrent candida – Swab – Treat ?? – Oral fluconazole?? – GBS – current practice Case 4 Antenatal • Mrs D • 16 weeks pregnant • Nasal congestion, coloured nasal discharge, frontal headache, 5 days. Temp 37.9 aural • 2 year old has streaming nose and moist cough • Mrs D desperate, can’t sleep, miserable +++ Options – limited guidelines • “Safe” remedies: saline • Unclassified but low risk remedies, eg topical decongestants (xymetolazone) • Nasal steroids –mometasone, fluticasone lowest systemic bioavailability, listed as B3, budesonide cat A • Antibiotics – amoxycillin, erythromycin cat A A, B, C, D, X – NOT hierarchical • Human data are lacking or inadequate for drugs in the B1, B2 and B3 categories • Subcategorisation of the B category is based on animal data • The allocation of a B category does not imply greater safety than a C category • Medicines in category D are not absolutely contraindicated during pregnancy (e.g.anticonvulsants) Case 5: Post partum • Nikki, with 3 day old Arthur calls from home • NVD, early discharge • Increasing “period pain” feeling hot and cold, moderate PV bleeding, light headed and tired • Midwife already visited for the day • Issues for GP: – ?how urgent – How to fit in to schedule – Who to call and how if concerned Cont. • Nikki attends the surgery as an urgent “fit in.” • Delivery record indicates placenta complete • O/E temp 38.2, uterus 3cm above pubic bone, mildly tender. BP normal, HR 85 – Empirical treatment – Investigation – swab – When to US? – When to send back to hospital? Summary - Immunisation • Immunise prepregnancy where possible • Live vaccines given in pregnancy are unlikely to be harmful • Influenza vaccine is routinely recommended for all pregnant women • dTpa is recommended pre-pregnancy, elsewhere used during pregnancy. – WATCH THIS SPACE • Hep B • Consider measles Summary - screening • New guidelines – HIV, hep B, syphillis, rubella, bacteriuria, chlamydia in <25s, Hep C if high risk, varicella if no history • Effective interventions available for all except Hep C • Parvovirus - case by case • GBS ??? Summary - infections • Diagnosis and treatment of non pregnancy related illness generally similar to non pregnant • Symptomatic treatments often safe and highly significant to women • Antibiotics category A first line if required Referral pathways • • • • Pre-conception or early pregnancy Antenatal Post partum Infectious diseases THANK YOU