PowerPoint
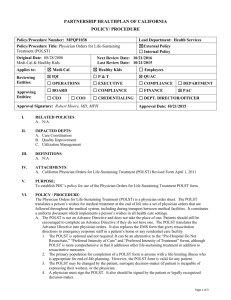
advertisement

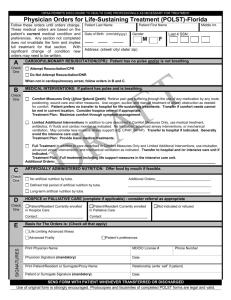
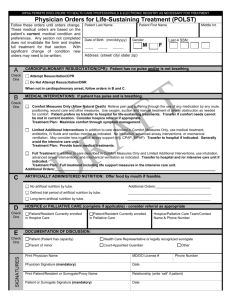
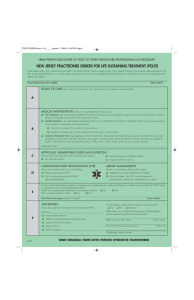
Disability Rights Leadership Institute on Bioethics April 25-26, 2014 Arlington, Virginia NOT DEAD YET Diane Coleman, JD, President/CEO 497 State Street Rochester, New York 14608 (585) 697-1640 www.notdeadyet.org Euthanasia Blues – Video By Norm Kunc http://www.youtube.com/watch?v=8Mwj8TUrbW g Pre-History & Formation of Not Dead Yet (NDY) Pre-History & Formation of Not Dead Yet (NDY) Elizabeth Bouvia – Early “Right to Die” Case Age 26, Cerebral Palsy Setbacks: Miscarriage, Marriage Breakup Vocational Rehab Agency took back van Forced to quit masters program Sought medical help for starvation with morphine Court equated her with terminally ill person Pre-History & Formation of NDY Fighting for the right to home care and freedom from nursing facilities in 1980’s, “Give Me Liberty or Give Me Death” Cases: David Rivlin Kenneth Bergstedt Larry McAfee ADAPT helped McAfee get out of a nursing home and he changed his mind. Pre-History & Formation of NDY A Name from a Movie: Monty Python and the Holy Grail Not Dead Yet founded April 27, 1996 Withholding & Withdrawal of Life Sustaining Treatment Ensuring that health care decisions are voluntary and based on informed consent, not pressured Ensuring that surrogate decisions are consistent with the person’s wishes and their civil rights Opposing involuntary, unilateral decisions by doctors, hospitals and other providers (aka futility policies) Surrogate decisions to withhold or withdraw life-sustaining treatment Surrogate Decision-Making Withholding or Withdrawing LifeSustaining Treatment based on the decision of: A surrogate chosen by individual A surrogate designated under a statutory scheme or appointed by a court Treatment Withholding: Surrogate Decisions – Landmark Case U.S. Supreme Court 1990 Cruzan decision – Surrogate may decide to withdraw treatment Food & water by tube = medical treatment that can be withdrawn State law determines details Pennsylvania case – In re David Hockenberry Age 53, intellectual disability Resided in Edensburg Center most of his life Got aspiration pneumonia Dec. 2007 Hospitalized, where doctors treated him with mechanical ventilation for several weeks Parents turned to the courts to establish their authority to refuse the ventilator and other treatments – court denied parents’ request He improved and no longer needed ventilator Pennsylvania Case - Hockenberry From the Pennsylvania Supreme Court decision: “We hold that where, as here, life-preserving treatment is at issue for an incompetent person who is not suffering from an endstage condition or permanent unconsciousness, and that person has no health care agent, the Act mandates that the care must be provided.” IN RE D.L.H., 2 A.3d 505 (2010). Wisconsin Case 13-year-old boy with I/DD had pneumonia Easily treatable by antibiotics His long-term facility was providing the antibiotics Doctor encouraged parents to transfer him to UW hospital so that he could be taken off of antibiotics, artificial nutrition and hydration. Boy then transferred to hospice care, where he died after being administered morphine. NDY partnering with ASAN on an Amicus Brief in Wisconsin case Disability Rights Wisconsin, the designated protection and advocacy agency for people with disabilities in Wisconsin, has filed suit against the University of Wisconsin Hospital and Clinics, and six physicians including Dr. Norman Fost, to prevent them from denying life-sustaining medical treatment to people with developmental disabilities. NDRN - Devaluing People with Disabilities: Medical Procedures that Violate Civil Rights [T]here are times . . . where physicians recommend and family or other surrogate decision makers decide to not provide a needed transplant, to withhold medical treatment including hydration and nutrition of individuals without a terminal condition, or to sterilize people all on the basis of their disabilities. Applied in these ways, medical decision making and procedures are discriminatory and deny basic constitutional rights to individuals with disabilities . . .. “Rush to Judgment” cases Haleigh Poutre: From “end of life” to “recovery” Massachusetts case of 11-year-old girl injured by parental abuse Withdrawal of a feeding tube sought by the state less than two weeks post-injury Abusive father went to court to keep feeding tube (to avoid murder charges against himself) State legal papers described her as almost “brain dead” The judge in the case ruled that Poutre should "pass away with dignity” (2008) The day after the ruling the news was released that Poutre had clearly recovered some level of consciousness Poutre was transferred to rehabilitation American Academy of Neurology Practice Parameters re PVS Diagnostic standard for establishing a persistent vegetative state. The vegetative state . . . is defined as being persistent at 1 month. . . . PVS can be judged to be permanent 12 months after traumatic injury. PVS can be judged to be permanent for nontraumatic injury after 3 months. The chance for recovery after these periods is exceedingly low . . .. Rush to Judgment – Studies show misdiagnosis of PVS Andrews, Murphy, Munday and Littlewood, Misdiagnosis of the vegetative state: retrospective study in a rehabilitation unit, British Medical Journal 1996;313:13-16 (6 July) Outcome Measure: Patients who showed an ability to communicate consistently using eye pointing or a touch sensitive single switch buzzer. Results: Of the 40 patients referred as being in the vegetative state, 17 (43%) were considered as having been misdiagnosed; seven of these had been presumed to be vegetative for longer than one year, including three for over four years. Rush to Judgment – “Window of Opportunity” “Reliable information about the character of an injured persons future may be especially hard to find at those times during the course of treatment when there may be a ‘convenient’ window of opportunity to stop interventions and allow the patient to die.” Nelson, Frader, “Brain Trauma and Surrogate Decisionmaking: Dogmas, Challenges and Response”, J Clin Ethics, Winter 2004, 15(4): 264-76. Rush to Judgment – Dr. J. Fins “Once a patient progresses to minimal consciousness, we can’t predict what’s going to happen,” says Dr. Joseph J. Fins, chief of medical ethics at Weill Cornell Medical College and author of a coming book, “Rights Come to Mind: Brain Injury, Ethics and the Struggle for Consciousness.”. . . . A Drug That Wakes the Near Dead, NYTimes Magazine, Jeneen Interlandi, Dec 1, 2011 Rush to Judgment It is not uncommon for doctors to assume the worst and advise family members to withdraw care early. They do so in part because they see their duty as helping loved ones face reality. But Fins argues that this is a cop-out. “It’s glossing over all the unknowns for the sake of a quicker, cleaner solution,” he says. “It’s wrong to be so uniformly fatalistic so early on, especially with all the data emerging about the prospects for later-stage recovery.” (Emphasis added.) A Drug That Wakes the Near Dead, NYTimes Magazine, Jeneen Interlandi, Dec 1, 2011 Organ procurement & transplantation policies Two Issues: Organ Procurement & Transplantation Network (OPTN) OPTN’s failure to protect individuals and families from being contacted and even pressured by organ procurement organizations (OPOs) prior to a decision that life support will be withdrawn OPTN's failure to establish protocols to ensure that organs are not procured before a conscious potential donor has received appropriate psychological counseling and support to live Section 2.8 Requirements for Controlled Donation after Circulatory Death (DCD) Protocols On Nov. 11-12, 2013, OPTN’s Board voted that, “Prior to the OPO [organ procurement organization] initiating any discussion with the legal next-of-kin about organ donation for a potential DCD donor, the OPO must confirm that the legal next-of-kin has elected to withdraw life sustaining medical treatment.” [Legal next-of-kin is defined to include a patient who is conscious and on a ventilator.] U.S. Dept. of Health and Human Services Should: 1. Take steps to ensure that OPTN carries out its responsibility to monitor and discipline organ procurement organizations. 2. Support counseling for people who acquire severe disabilities. Discrimination in eligibility for organ transplants: Amelia’s story From “Brick Walls”, by Chrissy Rivera: “I am going to try and tell you what happened to us on January 10, 2012, in the conference room in the Nephrology department at Children’s Hospital of Philadelphia. . . . We are in the year 2012 and my child still does not have the right to live, the right to a transplant, because she is developmentally delayed.” Discrimination in eligibility for organ transplants: Amelia’s story Following a national petition drive and negative publicity, the hospital’s position changed. "As an organization, we regret that we communicated in a manner that did not clearly reflect our policies or intent and apologize for the Riveras' experience," said Michael Apkon, senior vice president and chief medical officer. He added: "While we can unequivocally state that we do not disqualify transplant patients on the basis of intellectual ability... this event underscores the importance of our responsibility to effectively communicate with families.“ USA Today, 2-15-12: ASAN Policy Paper & Toolkit Organ Transplantation and People with I/DD: A Review of Research, Policy and Next Steps Organ Transplantation and People with Disabilities: A Toolkit for State Advocates www.autisticadvocacy.org “Futility” and “Futile Care” policies What is futility? State statute or medical provider policy “Doctor knows best” in treatment withholding Overrules patient decision, family decision Denies life-sustaining treatment based on -medical predictions (often unreliable) -quality of life judgments (often biased) 3 Types of Futility Statutes Requires continued treatment pending transfer by physician who judges treatment futile or otherwise protects (AL, FL, ID, KS, MD, MA, MN, NH, NY, OH, OK, WY ) Requires continued treatment for a limited time (two states, VA and TX) Allows or (vague) may allow physicians to act on futility judgments and withdraw treatment, non-specific about efforts that must be made to transfer patient first (the other states) Texas Futility Statute: “If the patient or the person responsible for the health care decisions of the patient is requesting life-sustaining treatment that the attending physician has decided and the review process has affirmed is inappropriate treatment,…The physician and the health care facility are not obligated to provide lifesustaining treatment after the10th day after the written decision…” Tex. Code Ann. § 166.046 (Vernon 2004). Oklahoma has legislation entitled the "Nondiscrimination in Treatment Act” A health care provider shall not deny to a patient a lifepreserving health care service the provider provides to other patients, the provision of which is directed by the patient or a person authorized to make health care decisions for the patient: 1. On the basis of a view that treats extending the life of an elderly, disabled, or terminally ill individual as of lower value than extending the life of an individual who is younger, non-disabled, or not terminally ill; or 2. On the basis of disagreement with how the patient or person authorized to make health care decisions for the patient values the tradeoff between extending the length of the patient's life and the risk of disability. NDY Texas Proposal for Ethics Committee Accountability Composition: At least one quarter non- hospital staff Must include members of both disability and aging advocacy organizations An independent oversight committee to adjudicate when individuals or families are in conflict with decision of ethics committee Slogan: “End the UNethics Committees” Physician/Medical Orders on LifeSustaining Treatment (POLST/MOLST) POLST: Having the POLST Conversation (Video) An example of a POLST conversation that conveys bias against living with disabilities: UC Davis Center for Healthy Aging – Physician Orders for Life-Sustaining Treatment (POLST):Honoring Patients’ Wishes for Treatment http://www.ucsd.tv/searchdetails.aspx?showID=18360&subject=health Concerns About POLST/MOLST Using POLST With Non-Terminal People Bias Against Life-Sustaining Technologies POLST Form May Not Reflect Person’s Wishes, but the doctor’s Lack of Independent Research on POLST Medical Professionals Not Held Accountable The Risk of Over-Interpretation of POLST Orders http://www.notdeadyet.org/full-written-publiccomment-disability-related-concerns-aboutpolst POLST is often overused Example: In Maryland, facilities have a duty to complete the MOLST form for residents of nursing homes, assisted living programs, kidney dialysis centers, home health agencies and hospices. Hospitals must complete the form for patients who will be transferring to such facilities or to another hospital. Does POLST Require Individual’s or Authorized Surrogate’s Signature? States that require patient/surrogate signature: CA, CO, GA, HI, ID, IL, IN, IA, LA, MT, NC, NV, NJ, PA, RI, UT, WA and WV States that don’t: MD, MN, NY, OR, TN and VT Source: ABA Commission on Law and Aging, POLST Program Legislative Comparison (2014) Second Thoughts CT Negotiated a POLST We Can Live With For person at end stage of serious illness Advisory group includes disability advocates Signature of patient or surrogate required Discussion involves methods for presenting choices for “end-of-life” care without steering patients toward particular options Discussion includes fully informing patients about both the benefits and risks of entering an immediately effective medical order for life sustaining treatment NOT DEAD YET: CENTRAL THEMES & MESSAGES Nothing About Us Without Us!!!!! Financial constraints pose a threat in the medical system. The medical system resists accountability. Bias against people with disabilities permeates society and medical providers. “Fear and loathing” of disability drives proeuthanasia advocacy.