Case Study: Gastrointesophageal Reflux Disease
Brian Byrne
Jeff Caprez
1.
How is acid produced and controlled within the gastrointestinal tract? a.
Acid specifically hydrochloric acid is produced in the stomach by parietal cells. These parietal cells are signaled by gastrin to produce hydrochloric acid. The inner layers of the stomach produce gastrin when food enters.
Pitts, J. What Causes Too Much Stomach Acid? Health Guidance.
September 11, 2013, from http://www.healthguidance.org/entry/12512/1/What-Causes-Too-
Much-Stomach-Acid.html
.
2.
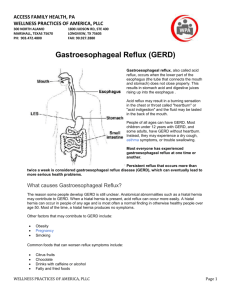
What role does lower esophageal sphincter (LES) pressure play in the etiology of gastroesophageal reflux disease? What factors affect LES pressure? a.
The LES is the sphincter that prevents stomach acid from entering the esophagus. When this sphincter relaxes, stomach acid can enter the esophagus and irritate it. Alcohol use can affect LES pressure by its depressant effects. Weight, sleeping habits, exercise habits, and smoking all put excess pressure on the LES and cause it to wear out.
De Giorgi, F. 2006, October, 26. Pathophysiology of gastrooesophageal reflux disease. Acta Otorhinolaryngologica Italica.
September, 11, 2013, from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2639970/.
3.
What are the complications of gastroesophageal reflux disease? a.
If GERD persists, esophagitis and Barrett’s esophagus can both occur.
Esophagitis is the inflammation and bleeding ulcers that can occur after prolonged exposure to stomach acid. Scar tissue can also grow constricting the elasticity of the esophagus, which can cause swallowing problems. Finally Barrett’s esophagus is where the epithelial cells of the esophagus change and can eventually lead to cancer.
2012, April, 30. Heartburn, Gastroesophageal Reflux (GER), and
Gastroesophageal Reflux Disease (GERD). National Digestive Diseases
Information Clearinghouse (NDDIC). September 11, 2013 from http://digestive.niddk.nih.gov/ddiseases/pubs/gerd/.
4.
The physician biopsied for H. pylori. What is this? a.
H. pylori is a bacterium that causes peptic ulcers in the stomach and sometimes the esophagus. Not all those infected with H. pylori however have ulcers.
2012, April, 30. H. pylori and Peptic Ulcers, National Digestive
Diseases 11, 2013
Brian Byrne
Jeff Caprez from http://digestive.niddk.nih.gov/ddiseases/pubs/gerd/.
5.
Identify the patient’s signs and symptoms that could suggest the diagnosis of gastroesophageal reflux disease a.
The main and only symptom exhibited by the patient is a burning sensation in the chest commonly referred to as heartburn. However there are a few other symptoms such as nausea and an inability to swallow.
2011, August, 11. Gastroesophageal Reflux Disease. PubMedHealth.
Semptember 11, 2013 from http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0001311/#adam_
000265.disease.symptoms.
6.
Describe the diagnostic tests performed for this patient. a.
Hematology is just the study of blood. This involves taking a blood sample and looking at the results of various cells in the blood. Chem
24 is similar to a complete blood count. The 48-hour pH monitoring checks the pH of the stomach acid and makes sure it is not too acidic.
The barium esophagram involves the patient swallowing barium sulfate and a radiologist then observes the reflux action due to the barium showing up on imaging.
Health Library. Johns Hopkins Medicine. 11, September, 2013 from http://www.hopkinsmedicine.org/healthlibrary/test_procedures/gas troenterology/
7.
What risk factors does the patient present with that might contribute to his diagnosis? (Be sure to consider lifestyle, medical, and nutritional factors.) a.
The patient is obese which is a risk factor for GERD. His diet especially with the high fatty foods and the excess of carbonated and alcoholic drinks are all risk factors with GERD. He also claimed to consume pizza or fried foods 1-2 times a week which with the tomato based food can increase risk.
2012, April, 30. Heartburn, Gastroesophageal Reflux (GER), and
Gastroesophageal Reflux Disease (GERD). National Digestive Diseases
Information Clearinghouse (NDDIC). September 11, 2013 from http://digestive.niddk.nih.gov/ddiseases/pubs/gerd/.
8.
The MD has decreased the patient’s does of daily aspirin and recommended discontinuing his ibuprofen. Why? How do aspirin and NSAIDs affect gastroesophageal disease? a.
This is due to the fact that aspirin and NSAIDs can increase the risk for ulcers and potentially cause them. This along with the wear and tear of GERD and GER can be a dangerous mix and cause bleeding ulcers.
Brian Byrne
Jeff Caprez
2012, April, 30. H. pylori and Peptic Ulcers, National Digestive Diseases
Information Clearinghouse (NDDIC). September 11, 2013 from http://digestive.niddk.nih.gov/ddiseases/pubs/gerd/.
9.
The MD has prescribed omeprazole. What class of medication is this? What is the basic mechanism of the drug? What other drugs are available in this class? What other groups of medications are used to treat GERD? a.
Omeprazole is a proton pump inhibitor. This class of drug inhibits the proton pump, which slows down the amount of hydrogen ions that are transferred across a boundary. Esomeprazole and Pantoprazole are both similar drugs in this class. Antacids and beta blockers are also used to treat GERD
January, 15, 2013. Omeprazole. MedlinePlus. September 11, 2013 from http://www.nlm.nih.gov/medlineplus/druginfo/meds/a693050.html
10.
Summarize the current recommendations for nutrition therapy. a.
We would recommend him to reduce his BMI and get him to a healthy weight to reduce his risk of CVD through a structured dietary plan that restricts alcohol consumption, intake of fried calorie dense foods, and reduce the overall cholesterol intake.
Academy of Nutrition and Dietetics. 2013. International Dietetics &
Nutrition Terminology Reference Manual. September 11, 2013.
11.
Calculate the patient’s %UBW and BMI. What does this assessment of weight tell you? In what ways may this contribute to his diagnosis? a.
The patient’s BMI is 31.82 and his %UBW is 119%. This assessment shows us that the patient has gained an immense amount of weight.
This can contribute to his diagnosis in that it places unnecessary strain on the LES and can cause it to loosen over time, thereby increasing GERD.
Weight(kg)/height^2(m)=BMI
Actual Weight/Usual Weight*100=%UBW
12.
Calculate energy and protein requirements for Mr. Nelson. How would this recommendation be modified to support a gradual weight loss? a.
The patient requires approximately 2700 calories. However he has been taking in more than 4400 calories according to his diet recall. His protein recommendation is approximately 100 grams however he is taking in 30 more grams than necessary. We would recommend slowly decreasing his calories. First week we would recommend a decrease to 4000 calories. Following week to 3600. And so on with a
Brian Byrne
Jeff Caprez
400 calorie drop each week until Mr. Nelson is around 2500 to 2600 calories to initiate weight loss.
13.
Complete a computerized nutrient analysis for this patient’s usual intake and
24-hour recall. How does his caloric intake compare to your calculated requirements?
Macronutrient Total (grams) Percentage of daily caloric intake
Fat 142.8
Carbohydrate 658.7
28.7%
58.8%
Protein 133.3
11.9% a.
Our calculated requirements are much lower than Mr. Nelson’s actual calorie intake.
14.
Are there any other abnormal labs that should be addressed to improve Mr.
Nelson’s overall health? Explain. a.
All of Mr. Nelson’s lipid levels were abnormal and should be addressed. His cholesterol, LDL, LDL/HDL ratio, and triglycerides were all too high and his HDL was too low. These should be addressed because Mr. Nelson has a family history of CAD with his father and while he is not experiencing problems yet, he very well could in the near future.
15.
What other components of lifestyle modification would you address in order to help in treating his disorder? a.
We would encourage Mr. Nelson to take up a new exercise regime perhaps on an arm cycle machine until his knee is healthy enough for his old routine. We would also encourage him to plan out his meal plan for the week every week so as to not eat out as much.
16.
Identify pertinent nutrition problems and corresponding nutrition diagnoses and write at least two PES statements for them. a.
Excessive Calorie Intake (NI 1.3) related to poor diet choices as evidenced by BMI of 31.82 and 24 hour diet recall b.
Excessive Fat Intake (NI 5.6.2) related to poor diet choices as evidenced by BMI of 31.82, 24 hour diet recall, and lipid profile of poor cholesterol levels.
Brian Byrne
Jeff Caprez c.
Nutrition knowledge deficit (NB 1.1) related to inability to determine which foods cause GER as evidenced by patient’s diet and symptoms
17.
Determine the appropriate intervention for each nutritional diagnosis. a.
We would encourage Mr. Nelson to learn more about his diagnosis and understand which foods may help or hurt his GERD. We also encourage Mr. Nelson to begin a healthier diet with
18.
Using Mr. Nelson’s 24-hour recall, outline necessary modifications you could use as a teaching tool. a.
The biggest concern was his intake of soda. Mr. Nelson would drink 5-
6 sodas a day, which was probably increasingly his likelihood of his
GERD acting up. Another concern was the amount of meals he had
“going out”. This no doubt limited his ability to consume healthier foods.