Respiratory Failure
advertisement

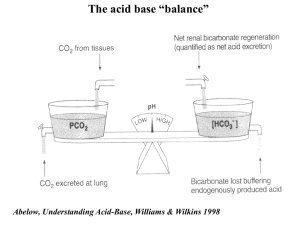
Chapter 11 Respiratory Failure §1 Concept and Introduction Respiration: a process concerned with gas exchange between a body and its environment. • External respiration • Transport of gas in blood • Internal respiration External respiration • Ventilation • Gas diffusion • Ventilation / Perfusion=4L/min ∕ 5L/min (VA/ Q = 0.8) PaO2: 80~100mmHg〔(13.3–0.043×age±0.06)〕 ×7.5 PaCO2: 40±0.5mmHg 1mmHg=0.133kPa 1kPa=7.5mmHg Respiratory Failure & Respiratory Insufficiency • Respiratory Failure is a pathological process in which the external respiration dysfunction leads to an abnormal decrease of arterial partial pressure of oxygen with or without retention of carbon dioxide. it is generally defined as (a resting subject, breathing air at sea level) a PaO2 of 60mmHg (8KPa) or less with or without PaCO2 of 50mmHg ( 6.7KPa) or more, or, the presence of hypoxia with or without hypercapnia. If FiO2 at sea level is not 20%: Respiratory failure index(RFI)=PaO2/FiO2≤300 • Respiratory insufficiency §2 Classification of RF RF can classified in three ways according to its duration ,primary site, and blood gas 1. According to duration (1)Acute RF —developed over minutes to days, It develops too rapidly to allow prompt, complete compensation and results in acid- base imbalance along with hypoxemia. (2)Chronic FR —developed over months to years, allowing compensatory mechanisms to improve oxygen transport and to buffer respiratory acidosis. . 2.According to primary site (1) Central RF — caused by disorder of CNS (2)Peripheral RF — caused by disease of respiratory organs or cavity. 3.According to blood gas (1) Hypoxemic RF (GroupⅠ) — characterized by ↓ PaO2 without ↑ PaCO2 (N /↓),often comes from gasexchanging dysfunction (2) Hypercapnic RF (GroupⅡ) — characterized by both↓ PaO2 and ↑ PaCO2 ,often comes from the alveolar ventilation disorder . §3 Causes & Pathogenesis • The process of respiration requires the integrated links of (1)the central control mechanisms and the peripheral nervous system,(2)the thoracic cage and the respiratory muscles.(3)the upper airways and lower airways.(4)the pulmonary gas-exchange units and(5) the pulmonary circulation. Disruptions of any of these links may be Causes of respiratory failure. • The respiratory functions include (1) ventilation , (2)gas diffusion,(3)ventilation/perfusion, Disruptions of any of these functions may be Pathogenesis of respiratory failure. Pathogenesis of RF 1.Ventilatory Disorder (1)Restrictive ventilatory disorder • Disorder of activity of respiratory muscles: – Damage or depression of CNS: Disease of the brain stem ,/ Some drug overdose – Neuro-muscular disorders: Injury to the spinal cord ,/ Poliomyelitis ,/ Myasthenia gravis • Decreased in compliance of chest wall and lungs compliance≈ distensibility C=dV/dP Volume ↓, Stiffness ↑ C ↓ Causes: Scoliosis ,/ Fibrothorax ,/ Pneumonectomy , / Pulmonary edema ,/ Surfactant ↓ • Pneumothorax and Hydrothorax (2)Obstructive ventilatory disorder • Central airway obstruction Diameter>2mm, – Fixed or variable narrowing or stenosis : Dense scars ,/ Foreign body aspiration ,/ Sputum /external compression. Variable extrathoracic obstructionInspiratory dyspnea Variable intrathoracic obstrucdtionExpiratory dyspnia • Peripheral airway obstruction Diameter<2mm, Intrinsic caliber ↓--Chronic bronchitis, / Bronchospasm, / Emphysema ( Chronic obstructive pulmonary disease ;COPD). Equal pressure point shifts up and Dynamic compression --- Expiratory dyspnea, Small airway closure • Change of the blood gas in ventilatory disorders 1. PaO2 ↓ + PaCO2↑,(GroupⅡ) ∆PaCO2↑/∆PaO2↓ ≈ respiratory quotient (R) ≈0.8 2. P(A-a)O2=normal (2~5mmHg) PaCO2=PACO2=0.863 ×VCO2 ∕ VA VA=4L/min PaCO2=40mmHg VA=2L/min PaCO2=80mmHg PaO2≈PAO2=PiO2 - PACO2 / R VA=4L/min PaO2=150-40 / 0.8=100mmHg VA=2L/min PaO2=150-80 / 0.8=50mmHg ∆PaCO2↑ ∕ ∆PaO2↓=40 ∕ 50=0.8 2. Diffusion impairment normal disorder • Total alveolar surface 80m2(72) < 40m2(35) • Alveolar-capillary membrane <1μm ↑ thickness or <5μm • Diffusing capacity of gas O2: 0.25s ↓ and Time of blood flow(0.75s) CO2: 0.07s Diffusing capacity of CO2>Diffusing capacity of O2 (20 times) Change of blood gas : PaO2 ↓, PaCO2 N ∕ ↓. (GroupⅠ) P(A-a)O2>2~5mmHg 3.Ventilation-Perfusion mismatching VA Q VA ∕ Q apex of lung base of lung total lung VA ∕ Q ≈ 0.8 P(A-a)O2=2~5mmHg 3 0.6 (1) VA↓ ∕ Q(N) ﹤ 0.8(0.1), ,Functional shunt , Venous admixture Causes: Bronchial asthma,/Chronic bronchitis,/ Obstructive aero- emphysema,/Pulmonary edema, /Fibroid lung. (2) VA(N) ∕ Q↓﹥0.8(10),Dead space like ventilation Causes: Pulmonary artery hypotension,/ Pulmonary artery embolism,/ DIC in lung. VD ∕ VT=30%60~70% (3) VA≈0 ∕ Q(N), Anatomical shunt ,True shunt Causes: Pulmonary artery-vein fistula,/ Pulmonary collapse,/Pulmonary consolidation Alteration of blood gas: PaO2↓, PaCO2 N/↓ (GroupⅠ) [ When total ventilation ↓ PaO2↓+PaCO2↑ (GroupⅡ) ] Mechanism : • Intact lung hyperventilation • Characteristic of the CO2 dissociation curve ---- line and the O2 dissociation curve----- S-shaped Acute respiratory distress syndrome (ARDS) • Concept: Many etiological factorssevere lung injury (alveolarcapillary membrane ) acute respiratory failure ( groupⅠ) §3 Alteration of function and metabolism 1.Disorders of acid-base and electrolyte (1) PaCO2↑Respiratory acidosis Hyperkalemia, Hypochloremia (2)PaO2↓ Metabolic acidosis Hyperkalemia, Hyperchloremia (3)PaCO2↓Respiratory alkalosis Hypokalemia, Hyperchloremia The mixed acid-base disturbances are usually present in the patient with RF. 2. Alteratino of respiratory system PaO2↓ hypotonic hypoxia carotid body - + respiratory centrer respiratory centrer (Peripheral chemoreceptor) PaO2 centrer (-) centrer(+) 30 PaCO2 60 centrer(+) 50 VA=2L/min PaO2=50 centrer(-) 80 PaCO2=80 Controlled oxygen therapy • GroupⅠ oxygen concentration<50% • GroupⅡ oxygen concentration<30% ,1~2L/min PaO2: 50~60mmHg Caused diseases Hypopnea,/Periodic respiration,/ Sighing respiration/Tidal respiration,/ Inspiratory dyspnea ,/ Expiratory dyspnea. 3.Alteration of cardiovascular system mild PaO2↓ heart rate↑,CO↑,Bp↑,redistribution of BF PaCO2↑ severe heart rate ↓,CO↓,Bp↓,cardiac arrhythmia pulmonary arteriolar constrictionpulmonary hypertentionRHF peripheral vasodilationwarm ,sweaty, flushed skin 4.Alteration of CNSPulmonary encephalopathy PaO2↓hypoxiaATP↓Na-K pump dysfunction acidosis of cerebral cells PaCO2↑cerebral vasodilation intracranial hypertention cerebral edema disturbances of cerebral cell metabolism 5. Altelation of renal function Acute renal dysfunction / failure 6.Altelation of GI Dysfunction of GI §4 Principles of Treatment 1. Treating the causes of respiratory failure 2. Increasing PaO2 3. Decreasing PaCO2 (1) Elimination of airway obstruction (2) Strengthening of respiratory drive (3) Mechanical ventilation 4. Treating the consequences of hypoxia and hypercapnia for example, the acidosis, heart failure etc.